Polymyxin B is a polymyxin antibiotic.
Uses
Systemic use of polymyxin B has, in most cases, been replaced by more effective and less toxic antibiotics for infections caused by susceptible organisms. However, polymyxin B may be useful in infections caused by organisms resistant to these drugs.
Polymyxin B sulfate has been used in the treatment of acute infections of the urinary tract or meninges, and of septicemia caused by susceptible strains of Ps. aeruginosa. The drug has also been used in the treatment of meningeal infections caused by H. influenzae, urinary tract infections caused by E. coli, and bacteremia caused by E. aerogenes and K. pneumoniae. Polymyxin B sulfate is not indicated for infections caused by Proteus or Neisseria species and should not be used for the treatment of minor infections or infections that can be successfully treated with less toxic antibiotics. Polymyxin B has been used orally to treat infections of the GI tract caused by Shigella and to treat diarrhea in infants caused by enteropathogenic E. coli; substantial evidence of effectiveness is lacking, however, and oral dosage forms are no longer available.
Polymyxin B sulfate in combination with neomycin sulfate is used for irrigation of the urinary bladder to prevent bacteriuria and bacteremia associated with the use of indwelling catheters. Bladder irrigation with the anti-infective combination appears to decrease the incidence of urinary tract infections when open drainage urinary catheter systems are used.
However, in one controlled study in patients with closed urinary catheter systems, bladder irrigation with the anti-infective combination did not decrease the incidence of bacteriuria compared to nonirrigation. Polymyxin B sulfate is used alone or in combination with other drugs such as other anti-infective agents and/or corticosteroids in the topical treatment of superficial infections of the skin caused by susceptible organisms; however, substantial evidence of effectiveness is lacking. Most experts question the use of topical antibiotics in general.
Reported clinical results often do not include controls. Minor skin infections and wounds usually heal without treatment, and systemic anti-infective therapy is usually required for the treatment of serious or extensive skin infections. Concomitant topical corticosteroids may mask the clinical signs of bacterial, fungal, or viral infections, preventing recognition of ineffectiveness of the antibiotic, or may suppress hypersensitivity reactions to substances in the product.
Dosage and Administration
Reconstitution and Administration
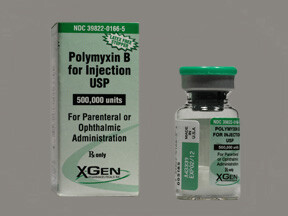
Polymyxin B sulfate is usually administered by IV injection. For the treatment of meningeal infections, the drug is given intrathecally. Although the drug may also be given IM, IM administration of polymyxin B sulfate should not be used routinely, particularly in infants and children, because of the severe pain which occurs at the injection site. If administered IM, IM injections should be given deeply into the upper outer quadrant of the gluteal muscles. For IV administration, polymyxin B sulfate is reconstituted by dissolving 500,000 units of the drug in 300-500 mL of 5% dextrose injection, to provide solutions containing approximately 1667 units to 1000 units of polymyxin B per mL. The drug is administered as an IV infusion, usually over a period of 60-90 minutes. For IM administration, the sterile powder is reconstituted by adding 2 mL of sterile water for injection, 0.9% sodium chloride injection, or 1% procaine hydrochloride injection to a vial labeled as containing 500,000 units of polymyxin B. The resultant solution contains approximately 250,000 units of polymyxin B per mL. For intrathecal administration, polymyxin B sulfate is reconstituted by adding 10 mL of 0.9% sodium chloride injection to a vial labeled as containing 500,000 units of the drug to provide a solution containing approximately 50,000 units/mL. Procaine hydrochloride should not be used in intrathecal injections.
Dosage
Potency and dosage of polymyxin B sulfate are expressed in terms of polymyxin B activity. The usual IV dosage of polymyxin B for adults and children older than 2 years of age is 15,000-25,000 units/kg daily if renal function is normal. The drug may be administered in divided doses every 12 hours. The total daily IV dose in these patients should not exceed 25,000 units/kg. Infants with normal renal function can receive up to 40,000 units/kg IV daily. The usual IM dosage of polymyxin B for adults and children older than 2 years of age with normal renal function is 25,000-30,000 units/kg daily administered in divided doses at 4- to 6-hour intervals. Infants with normal renal function may receive up to 40,000 units/kg daily. In limited clinical studies, up to 45,000 units/kg daily has been used in premature and full-term neonates for the treatment of sepsis caused by Ps. aeruginosa.
The usual intrathecal dosage of polymyxin B for adults and children older than 2 years of age is 50,000 units once daily for 3 or 4 days. The frequency of doses should then be reduced to once every other day for at least 2 weeks after cultures of the CSF are negative for bacteria and normal for glucose content. The usual intrathecal dosage of polymyxin B for children younger than 2 years of age is 20,000 units once daily for 3 or 4 days, or 25,000 units once every other day. With either regimen, therapy should be continued with 25,000 units once every other day for at least 2 weeks after cultures of the CSF are negative for bacteria and normal for glucose content. For continuous irrigation of the urinary bladder, 1 mL of the commercially available urogenital concentrate containing 200,000 units of polymyxin B and 57 mg of neomycin sulfate is added to 1 L of 0.9% sodium chloride solution and administered via a 3-way catheter at the rate of 1 L every 24 hours (approximately 40 mL/hour). If the patient’s urine output exceeds 2 L/day, the manufacturer recommends that the inflow rate be adjusted to 2 L every 24 hours. Duration of irrigation therapy should not exceed 10 days. Total systemic administration and topical application of polymyxin B should not exceed 2 million units daily for adults; in general, total systemic administration and ophthalmic instillation should not exceed 25,000 units/kg daily.
Dosage in Renal Impairment
In patients with impaired renal function, serum polymyxin B concentrations should be determined and IV or IM dosage should be adjusted to maintain desired serum concentrations whenever possible. Various methods have been used to estimate dosage requirements when serum concentrations are not known. In one method, it has been suggested that patients with creatinine clearances greater than 20 mL/minute may be given 75-100% of the usual daily dose in 2 divided doses every 12 hours and those with creatinine clearances of 5-20 mL/minute may receive 50% of the usual daily dose in 2 divided doses every 12 hours. Those with creatinine clearances of less than 5 mL/minute may receive 15% of the usual daily dose every 12-hours.
Cautions
Adverse Effects
Nephrotoxicity and neurotoxicity are the most serious adverse effects of parenteral polymyxin B sulfate therapy and are most likely to occur in patients receiving higher than recommended doses or in patients with impaired renal function unless dosage is reduced. Nephrotoxicity may be manifested by albuminuria, cylindruria, azotemia, hematuria, leukocyturia, excessive excretion of electrolytes, and rising drug blood concentrations without an increase in dosage.
Neurotoxicity is manifested by flushing of the face, dizziness, mental confusion, irritability, nystagmus, muscle weakness, drowsiness, giddiness, circumoral and peripheral paresthesia or numbness, blurring of vision, slurred speech, ataxia, coma, or seizures. In addition, respiratory paralysis may occur as a result of neuromuscular blockade, especially in patients with neuromuscular disease such as myasthenia gravis or in patients who are receiving neuromuscular blocking agents or general anesthetics. (See Drug Interactions.)
Drug-induced neuromuscular blockade is not easily reversed and is resistant to neostigmine and edrophonium; calcium chloride has been used successfully in some cases. Intrathecal administration of polymyxin B sulfate may cause meningeal irritation with headache, fever, stiff neck, and increased leukocytes and protein in the CSF. In addition, nerve root irritation may occur causing neuritic pain and urine retention. Fever, urticaria, skin exanthemata, eosinophilia, and anaphylactoid reactions with dyspnea and tachycardia have been reported rarely during parenteral polymyxin B therapy. Repeated IM injections are not recommended, because of the irritation and severe pain that commonly occur at the site of injection, particularly in infants and children.
Thrombophlebitis at IV injection sites has also been reported. Polymyxin B has a low order of toxicity when applied topically, and hypersensitivity reactions are rare. However, some commercially available combination products contain other ingredients such as neomycin and/or preservatives that frequently induce allergic contact dermatitis.
Precautions and Contraindications
Polymyxin B can cause potentially serious nephrotoxicity and/or neurotoxicity and should be administered for systemic use only under the constant supervision of a physician. Polymyxin B should be administered parenterally or intrathecally only to hospitalized patients who have received baseline renal function tests prior to treatment. Renal function and serum drug concentrations should be monitored frequently during therapy. In patients with impaired renal function or nitrogen retention, polymyxin B sulfate dosage should be reduced. If urine output diminishes, serum creatinine or BUN rises, or signs of respiratory paralysis appear during polymyxin B therapy, the drug should be discontinued. The use of polymyxin B sulfate may result in an overgrowth of nonsusceptible organisms including fungi. Appropriate therapy should be instituted if superinfection occurs. Polymyxin B is contraindicated in patients with a history of hypersensitivity to any of the polymyxins.
Pregnancy
The safety of polymyxin B in pregnant women has not been established. Polymyxin B should be used during pregnancy only when clearly needed.
Drug Interactions
Neuromuscular Blocking Agents and Anesthetics
Polymyxin B is believed to inhibit neuromuscular transmission. Parenterally administered polymyxin B may increase or prolong skeletal muscle relaxation produced by neuromuscular blocking agents and/or anesthetics if the antibiotic is administered during surgery, or may reinstate neuromuscular blockade if administered parenterally postoperatively; the concurrent use of these agents should be avoided. Concurrent use of polymyxin B with these agents may precipitate respiratory paralysis, and equipment for assisted respiration should be available if concomitant use of the drugs cannot be avoided.
Nephrotoxic and Neurotoxic Drugs
Since nephrotoxic and neurotoxic effects may be additive, concurrent and/or sequential use of systemic polymyxin B and other drugs (administered systemically, orally, or topically) with similar toxic potential (e.g., aminoglycosides, other polypeptide antibiotics, sodium citrate, parenteral quinine, parenteral quinidine) should be avoided, if possible. Mechanism of Action Polymyxin B sulfate is bactericidal. The drug binds to phosphate groups in the lipids of bacterial cytoplasmic membrane and acts as a cationic detergent, thereby altering the osmotic barrier of the membrane and causing leakage of essential metabolites.
Spectrum Polymyxin B sulfate’s spectrum of activity is similar to that of colistin derivatives. Polymyxin B is active in vitro against many gram-negative organisms; however, most species of Proteus and Neisseria are resistant to the drug, as are all gram-positive organisms and fungi. When the Kirby-Bauer disk-diffusion procedure is used for susceptibility testing, a 300-unit polymyxin B disk is used. When the Kirby-Bauer procedure is used, organisms with growth inhibition zones of greater than 11 mm are usually considered to be susceptible to polymyxin B. In vitro, polymyxin B concentrations of 0.5-15 mcg/mL inhibit most strains of Pseudomonas aeruginosa, 0.1-20 mcg/mL inhibit most Escherichia coli, 0.75-5 mcg/mL inhibit most Haemophilus influenzae, 0.02-10 mcg/mL inhibit most Enterobacter aerogenes, and 0.4-8 mcg/mL inhibit most Klebsiella pneumoniae.
For many susceptible organisms, the minimum bactericidal concentration of polymyxin B in vitro is 2-4 times the minimum inhibitory concentration. It appears that divalent cations (e.g., calcium in serum) antagonize the activity of polymyxin B against Ps. aeruginosa by preventing binding of the antibiotic to the bacterial cell membrane. As a result, the drug appears to be less active against Pseudomonas in vivo than in vitro. This effect has not been observed with other gram-negative organisms. A synergistic relationship has been demonstrated in vitro between carbenicillin and polymyxin B in the inhibition of some strains of Ps. aeruginosa. Synergism between polymyxin B and bacteriostatic antibiotics (e.g., tetracyclines, chloramphenicol, erythromycin, sulfonamides) in inhibiting various bacteria has also been reported. Resistance Infrequently, bacteria slowly develop varying degrees of resistance to polymyxin B.
There is complete cross-resistance between colistin derivatives and polymyxin B, but no reports have been published on cross-resistance between the polymyxins and other antibiotics.
Pharmacokinetics
Absorption
Polymyxin B sulfate is not absorbed from the GI tract, except in infants who may absorb up to 10% of a dose. After IM administration of a single dose of 20,000-40,000 units/kg in adults, peak serum concentrations of 1-8 mcg/mL are obtained within approximately 2 hours. Serum concentrations are higher in infants, probably because of less binding of the drug to cell membrane phospholipids. Following IM administration of polymyxin B to adults with normal renal function, detectable amounts of the drug are present in the serum for up to 12 hours. Serum concentrations are higher and more prolonged in patients with renal impairment. Data are not available on blood concentrations following IV administration and CSF concentrations following intrathecal administration. Polymyxin B does not appear to be absorbed to an appreciable extent from mucous membranes or intact or denuded skin.
Distribution
Polymyxin B is widely distributed into body tissues. The drug does not appear in the CSF (even when the meninges are inflamed) or synovial fluid and does not cross the placenta. Systemically administered polymyxin B does not penetrate into the aqueous humor of the eye, even in the presence of inflammation. Animal studies indicate that following IV or IM administration, approximately 50% of a dose is reversibly bound to phospholipids of cell membranes in the liver, kidneys, heart, muscle, brain, and probably other tissues. Polymyxin does not appear to be highly bound to serum proteins.
Elimination
The serum half-life of polymyxin B is reported to be 4.3-6 hours in adults with normal renal function. In patients with creatinine clearances of less than 10 mL/minute, the serum half-life of polymyxin B has been reported to be 2-3 days. Approximately 60% of a dose is excreted unchanged into the urine by glomerular filtration. Information is lacking on the fate of the other 40% of the dose. In adults, there is a 12- to 24-hour time lag following the initial dose during which very little polymyxin B appears in the urine, possibly as a result of binding of the drug to phospholipids of kidney cell membranes. Excretion continues for 24-72 hours after the final dose is administered. In adults with normal renal function, urinary drug concentrations average 20-100 mcg/mL following usual IM doses at 6-hour intervals over a period of a few days. Infants excrete polymyxin B faster than do adults; 40-60% of an administered dose is excreted within 8 hours in the urine. Polymyxin B is not removed to an appreciable extent by either hemodialysis or peritoneal dialysis.
Chemistry and Stability
Chemistry
Polymyxin B is one of several polymyxin antibiotics derived from various strains of Bacillus polymyxa. Polymyxin B sulfate occurs as a white to buff-colored, hygroscopic powder that is odorless or has a faint odor. The drug is freely soluble in water and in 0.9% sodium chloride injection and slightly soluble in alcohol. Polymyxin B sulfate contains not less than 6000 units of polymyxin B activity per mg, calculated on the dried basis, and each mg of pure polymyxin B is equivalent to 10,000 units of polymyxin B activity. Aqueous solutions of polymyxin B sulfate have a pH of 5-7.5.
Stability
Commercially available polymyxin B sulfate sterile powder should be protected from light and stored at a temperature less than 30°C. When stored under these conditions, the expiration date is 5 years following the date of manufacture. Aqueous solutions of polymyxin B sulfate having a pH of 5-7.5 can be stored for 6-12 months at 2-8°C without appreciable loss of potency; however, any unused portion of solutions intended for parenteral use should be discarded after 72 hours. The drug should not be stored in alkaline solutions since they are less stable. Polymyxin B sulfate is inactivated by strong acidic or alkaline solutions. The drug is chemically incompatible with many drugs including amphotericin B, cephalothin sodium (no longer commercially available in the US), chloramphenicol sodium succinate, chlorothiazide sodium, heparin sodium, nitrofurantoin sodium, penicillins, prednisolone sodium phosphate, and tetracyclines. Polymyxin B sulfate in solution is also incompatible with the salts of calcium and magnesium.
Preparations
Polymyxin B Sulfate Parenteral For injection 500,000 units (of polymyxin Polymyxin B Sulfate Sterile,B) Bedford Neomycin and Polymyxin B Sulfates Urogenital Concentrate, 57 mg Neosporin Sulfate (40 Neomycin and Polymyxin B sterile, for mg of neomycin) per mL and Sulfates Solution for irrigation Polymyxin B Sulfate 200,000 Irrigation, (preservative-free units (of polymyxin B) per in ampuls or with mL methylparaben in multiple-dose vials) Schein Steris Neosporin® G.U. Irrigant, (preservative-free in ampuls or with methylparaben in multiple-dose vials) GlaxoSmithKline

