Dicloxacillin Sodium, Nafcillin Sodium, Oxacillin Sodium, Preface to the General Statements on Penicillins
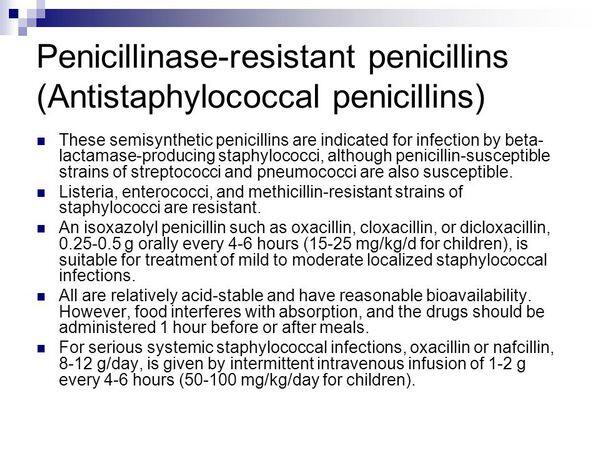
Penicillinase-resistant penicillins are semisynthetic penicillin antibiotics that are resistant to staphylococcal penicillinases.
Uses
Penicillinase-resistant penicillins are used in the treatment of infections caused by, or suspected of being caused by, susceptible penicillinase-producing staphylococci. Although penicillinase-resistant penicillins have been effective when used in the treatment of infections caused by other susceptible gram-positive aerobic cocci (e.g., Streptococcus pneumoniae, S. pyogenes, nonpenicillinase-producing staphylococci), the drugs are less active than natural penicillins against these gram-positive bacteria in vitro on a weight basis and should not be used in the treatment of infections caused by organisms susceptible to penicillin G and penicillin V. Penicillinase-resistant penicillins have been used for perioperative prophylaxis but are not considered drugs of choice for such prophylaxis.
Prior to initiation of therapy with a penicillinase-resistant penicillin, appropriate specimens should be obtained for identification of the causative organism and in vitro susceptibility testing. A penicillinase-resistant penicillin may be used empirically for the treatment of any infection suspected of being caused by susceptible staphylococci, but the drug should be discontinued and appropriate anti-infective therapy substituted if the infection is found to be caused by an organism other than a penicillinase-producing staphylococci susceptible to penicillinase-resistant penicillins. If staphylococci resistant to penicillinase-resistant penicillins (oxacillin-resistant staphylococci; previously known as methicillin-resistant staphylococci) are prevalent in the hospital or community, empiric therapy of suspected staphylococcal infections should include vancomycin.(See Oxacillin-Resistant Staphylococcal Infections in Uses: Staphylococcal Infections.) Penicillinase-resistant penicillins should not be used orally for the initial treatment of severe, life-threatening infections, including meningitis, but may be used as follow-up therapy after parenteral penicillinase-resistant penicillin therapy.
Staphylococcal Infections
Penicillinase-resistant penicillins are the drugs of choice for the treatment of infections caused by susceptible penicillinase-producing staphylococci. The drugs have been effective when used in the treatment of upper and lower respiratory tract infections, skin and skin structure infections, bone and joint infections,urinary tract infections, meningitis, bacteremia, and endocarditis caused by susceptible penicillinase-producing staphylococci. Penicillinase-resistant penicillins also are used in the management of infections related to peripheral vascular and central venous catheters. 270 Because the majority of clinical isolates of staphylococci, regardless of source, are resistant to natural penicillins, a penicillinase-resistant penicillin usually is indicated for initial treatment of infections suspected of being caused by staphylococci.
If a staphylococcal infection fails to respond to therapy with a penicillinase-resistant penicillin although in vitro tests indicate that the causative organism is susceptible to the drugs, the presence of undrained abscesses or perivascular infections should be considered. Anti-infective therapy alone rarely is effective for staphylococcal infections in individuals with undrained abscesses or with infected foreign bodies; surgical intervention may be necessary.
The possibility that the causative organism may be tolerant to penicillins or that the infection may be caused by oxacillin-resistant staphylococci also should be considered since routine in vitro susceptibility tests may not detect penicillin tolerance or resistance to penicillinase-resistant penicillins. (See Spectrum: In Vitro Susceptibility Testing.) Many clinicians suggest that serum bactericidal titers (SBTs) be used to monitor the adequacy of penicillinase-resistant penicillin therapy in patients with staphylococcal endocarditis or osteomyelitis and to adjust dosage of the drugs.
Although the value of SBTs has not been definitely established and there is a wide variation in SBTs depending on the method used, peak SBTs of 1:8 or greater in patients with staphylococcal endocarditis receiving a penicillinase-resistant penicillin generally have been associated with high cure rates. A peak SBT of 1:8 or greater also has been recommended when an oral regimen is used for the treatment of bone or joint infections; other clinicians suggest that SBTs in patients with osteomyelitis should be 1:16 or greater.
Osteomyelitis
Because acute osteomyelitis, especially in children, frequently is caused by penicillinase-producing S. aureus, a penicillinase-resistant penicillin usually is included in the empiric regimen pending results of in vitro tests. In neonates, the most frequent causes of osteomyelitis are S. aureus, S. agalactiae (group B streptococci), and gram-negative bacilli (e.g., Escherichia coli), and empiric therapy with a penicillinase-resistant penicillin and a third generation cephalosporin (e.g., cefotaxime) provides coverage against these organisms. In older infants and children through 5 years of age, the principal pathogens usually are S. aureus, streptococci, and H. influenzae, and many clinicians recommend empiric therapy with cefuroxime or a third generation cephalosporin (e.g., ceftriaxone, cefotaxime).
In adults and children older than 5 years of age, osteomyelitis usually is caused by S. aureus, and a penicillinase-resistant penicillin usually is recommended for empiric therapy in these age groups; however, if arthritis is present, other pathogens may be involved and a broad-spectrum anti-infective (e.g., cefuroxime, third generation cephalosporin) may be indicated unless gram-positive cocci are demonstrated in synovial fluid samples.
Many clinicians recommend that acute osteomyelitis in adults or children caused by susceptible penicillinase-producing staphylococci be treated with a parenteral penicillinase-resistant penicillin for 3-8 weeks. Alternatively, some clinicians recommend that a parenteral penicillinase-resistant penicillin be used initially followed by an oral penicillinase-resistant penicillin. In several controlled studies in children with acute osteomyelitis, penicillinase-resistant penicillin therapy was effective when the drugs were administered parenterally for 5-28 days or until the patient was afebrile for 3 consecutive days, then orally for 3-6 weeks or until the total duration of parenteral and oral therapy was at least 6 weeks.
For the treatment of chronic osteomyelitis caused by penicillinase-resistant staphylococci, many clinicians recommend treatment with a parenteral penicillinase-resistant penicillin given for at least 4-6 weeks followed by an oral penicillinase-resistant penicillin given for at least an additional 1-2 months. Chronic osteomyelitis also has been treated successfully with high dosages of oral dicloxacillin given for prolonged periods (6 months or longer) either alone or in conjunction with probenecid.
Endocarditis
IV nafcillin or IV oxacillin is used for the treatment of endocarditis caused by susceptible strains of S. aureus or S. epidermidis and are the drugs of choice for the treatment of endocarditis caused by penicillin-resistant staphylococci.
Because results of in vitro studies indicate that a b-lactam antibiotic used in conjunction with an aminoglycoside results in a more rapidly bactericidal action than the b-lactam antibiotic alone, some clinicians recommend that an aminoglycoside be used in conjunction with an IV penicillinase-resistant penicillin for the initial treatment of S. aureus endocarditis.
However, penicillinase-resistant penicillins have been effective when used parenterally alone for 4-6 weeks in the treatment of endocarditis caused by susceptible staphylococci and the relative efficacy of concomitant therapy compared with penicillin therapy alone has not been definitely established. Although concomitant therapy with a penicillinase-resistant penicillin and an aminoglycoside may result in accelerated bacteriologic and clinical responses compared with therapy with a penicillinase-resistant penicillin alone, such therapy does not appear to improve survival or reduce valvular damage and may be associated with an increased incidence of adverse effects.
Therefore, many clinicians recommend that treatment of staphylococcal endocarditis be initiated with concomitant therapy but that the aminoglycoside be discontinued after clearance of bacteremia (3-7 days) and the penicillinase-resistant penicillin continued alone for 4-6 weeks. Gentamicin is the aminoglycoside usually recommended for concomitant use with nafcillin or oxacillin for the treatment of staphylococcal endocarditis; however, if the strain is found to be resistant to gentamicin, another aminoglycoside should be substituted based on results of in vitro susceptibility testing. Endocarditis caused by S. lugdunensis tends to cause a more virulent form of endocarditis than other coagulase-negative staphylococci. Most experts recommend that endocarditis caused by S. lugdunensis be treated with standard anti-infective regimens based on in vitro susceptibility test results and that patients be monitored closely for periannular extension or extracardiac spread of the infection.
Native Valve Endocarditis
For the treatment of native valve endocarditis caused by staphylococci susceptible to penicillinase-resistant penicillins, the American Heart Association (AHA) recommends that adults and pediatric patients receive a 4- to 6-week regimen of IV nafcillin or IV oxacillin given with or without gentamicin. The AHA states that, although the benefits of concomitant aminoglycoside therapy have not been clearly established in these infections, gentamicin may be given concomitantly for the first 3-5 days of the penicillinase-resistant penicillin regimen. In those very rare cases when native valve endocarditis is caused by staphylococci susceptible to penicillin (penicillin MIC 0.1 mcg/mL or less), the AHA states that adults may receive a 4-6-week regimen of penicillin G sodium instead of nafcillin or oxacillin.
The AHA states that limited data suggest that a 2-week regimen of IV nafcillin or IV oxacillin given with an aminoglycoside may be effective in IV drug abusers who have right-sided endocarditis caused by susceptible S. aureus; however, this shorter regimen should not be used in IV drug abusers with evidence of metastatic infection or left-sided endocarditis (mitral or aortic murmur, systemic emboli or cutaneous stigmata, or echocardiographically demonstrated vegetations on mitral or aortic valves). In addition, it is unclear whether those with right-sided S. aureus endocarditis and echocardiographically demonstrated vegetations (tricuspid or pulmonic valve), underlying acquired immunodeficiency syndrome (AIDS), or extensive pulmonary complications of right-sided endocarditis (lung abscess) are appropriate candidates for the 2-week regimen.
For the treatment of native valve staphylococcal endocarditis in adults and pediatric patients with a history of penicillin hypersensitivity, the AHA recommends a regimen of IV cefazolin or other first generation cephalosporin (cephalosporins should be avoided in patients who have had an immediate-type hypersensitivity reaction to penicillins) given with or without IM or IV gentamicin during the first 3-5 days of therapy or, alternatively, a regimen of IV vancomycin. Native valve endocarditis caused by oxacillin-resistant staphylococci (previously known as methicillin-resistant staphylococci) usually is treated with a regimen of IV vancomycin.
Endocarditis in the Presence of Prosthetic Valves or Materials
For the treatment of endocarditis caused by staphylococci susceptible to penicillinase-resistant penicillins in adults and pediatric patients with prosthetic valves or other prosthetic material, the AHA recommends a regimen of IV nafcillin or IV oxacillin given with oral rifampin for 6 weeks or longer and with IM or IV gentamicin given for the first 2 weeks. However, coagulase-negative staphylococci causing prosthetic valve endocarditis usually are resistant to penicillinase-resistant penicillins (especially when endocarditis develops within 1 year after surgery) and, unless results of in vitro testing indicate that the isolates are susceptible to penicillinase-resistant penicillins, coagulase-negative staphylococci involved in prosthetic valve endocarditis should be assumed to be oxacillin-resistant. For the treatment of adults and pediatric patients with prosthetic valves or other prosthetic materials who have endocarditis caused by staphylococci resistant to penicillinase-resistant penicillins, the AHA usually recommends a combination regimen of IV vancomycin and oral rifampin given for 6 weeks or longer with IM or IV gentamicin given concomitantly during the first 2 weeks of therapy.
Infections Related to Intravascular Catheters
Penicillinase-resistant penicillins often are used for the empiric treatment of infections related to peripheral vascular and central venous catheters since these infections usually are caused by coagulase-negative staphylococci (e.g., S. epidermidis), S. aureus, aerobic gram-negative bacilli (e.g., Acinetobacter, Pseudomonas aeruginosa), or Candida albicans.
The Infectious Diseases Society of America (IDSA), American College of Critical Care Medicine, and Society for Healthcare Epidemiology of America recommend that the empiric regimen be chosen based on the severity of the patient’s clinical disease, risk factors for infection, and the most likely pathogens associated with the specific intravascular device.
Unless the hospital or area has a high incidence of oxacillin-resistant staphylococci, these experts recommend use of a penicillinase-resistant penicillin (nafcillin, oxacillin) for empiric therapy of catheter-related infections when S. aureus are suspected. If coagulase-negative staphylococci or oxacillin-resistant staphylococci are suspected, vancomycin should be used initially for empiric therapy but the regimen should be changed to a penicillinase-resistant penicillin if the causative organisms is found to be susceptible to the penicillins. In severely ill or immunocompromised patients who have suspected catheter-related bloodstream infections, a third or fourth generation cephalosporin (e.g., ceftazidime, cefepime) may be indicated to provide empiric coverage for gram-negative enteric bacilli and Pseudomonas aeruginosa.
Although IV therapy is indicated initially, an oral anti-infective regimen (e.g., oral ciprofloxacin, co-trimoxazole, linezolid) can be substituted once the patient’s condition stabilizes. It has been suggested that 10-14 days of anti-infective therapy may be sufficient for the treatment of uncomplicated catheter-related infections caused by S. aureus in immunocompetent patients without underlying valvular heart disease or an intravascular prosthetic device; however, 4-6 weeks of therapy may be necessary when there is persistent bacteremia after catheter removal or evidence of endocarditis or septic thrombosis and 6-8 weeks may be necessary when osteomyelitis is present.
The recommendations of the IDSA, American College of Critical Care Medicine, and Society for Healthcare Epidemiology of America should be consulted for more specific information on management of intravascular catheter-related infections, including information on how to obtain diagnostic cultures, indications for catheter removal, and use of local anti-infective lock therapy when the catheter is not removed.
Meningitis and Other CNS Infections
Nafcillin and oxacillin are used parenterally for the treatment of meningitis or ventriculitis caused by susceptible penicillinase-producing staphylococci. IV nafcillin is considered by many clinicians to be the preferred penicillinase-resistant penicillin for the treatment of CNS infections caused by susceptible penicillinase-producing staphylococci because of reportedly greater CSF penetration.
Oxacillin-Resistant Staphylococcal Infections
Because oxacillin-resistant staphylococci (ORSA; previously known as methicillin-resistant staphylococci or MRSA) are being reported with increasing frequency (see Resistance: Oxacillin-Resistant Staphylococci), initial therapy for suspected staphylococcal infections should include vancomycin if oxacillin-resistant strains are prevalent in the community or hospital. Oxacillin-resistant S. aureus are an important cause of nosocomial infections, especially in patients who are seriously ill, and also have been reported with increasing frequency in community-acquired infections.
Patients with lengthy hospitalizations, premature infants, and individuals with diabetes mellitus, peripheral vascular disease, or surgical or burn wounds are at particularly high risk of acquiring oxacillin-resistant S. aureus and these strains also have been reported frequently in patients with prosthetic valve endocarditis, intravascular catheters, infected CSF shunts, 247 dermatologic disorders, renal dysfunction, or human immunodeficiency virus (HIV) infection, and in granulocytopenic children with cancer. Infections caused by oxacillin-resistant S. aureus or S. epidermidis generally are treated with vancomycin alone or vancomycin in conjunction with rifampin and/or an aminoglycoside. (See Uses: Staphylococcal Infections, in Vancomycin Hydrochloride 8:12.16.08.)
Penicillin-Tolerant Staphylococcal Infections
Optimum anti-infective therapy for infections caused by penicillin-tolerant staphylococci has not been established. Because in vitro studies indicate that the bactericidal activity of aminoglycosides and b-lactam antibiotics may be additive or synergistic, some clinicians recommend that an aminoglycoside be used in conjunction with a penicillinase-resistant penicillin in the treatment of severe infections, especially endocarditis, caused by penicillin-tolerant penicillinase-producing staphylococci.
However, the value of concomitant therapy in the treatment of infections caused by penicillin-tolerant staphylococci has not been definitely established. Results of some studies in patients with endocarditis caused by penicillin-tolerant staphylococci indicate that concomitant therapy with an aminoglycoside and a penicillinase-resistant penicillin generally was no more effective than the penicillinase-resistant penicillin alone; however, a shorter time to defervescence occurred in patients receiving concomitant therapy.
Perioperative Prophylaxis
Penicillinase-resistant penicillins have been used for perioperative prophylaxis to reduce the incidence of infections in patients undergoing certain surgical procedures that are associated with a high incidence of staphylococcal infections, but are not considered drugs of choice for such prophylaxis. Although IV cefazolin usually is the drug of choice for perioperative prophylaxis in patients undergoing neurosurgical procedures (e.g., craniotomy, CSF shunting), some clinicians suggest that IV nafcillin or IV oxacillin (a single 1-g dose given at induction of anesthesia) may be used as an alternative.
Vancomycin is preferred in hospitals where staphylococci resistant to penicillinase-resistant penicillins frequently cause wound infection and is recommended for patients allergic to penicillins and cephalosporins. Nafcillin and oxacillin have been effective when used perioperatively to reduce the incidence of infection in patients undergoing cardiovascular or orthopedic surgery, including open heart surgery, total hip replacement, implantation of prosthetic material, or hip fracture repair. However, penicillinase-resistant penicillins are not generally recommended for perioperative prophylaxis in patients undergoing these procedures.
Many clinicians currently recommend IV cefazolin or IV cefuroxime for perioperative prophylaxis in patients undergoing cardiovascular surgery and IV cefazolin in patients undergoing orthopedic surgery; vancomycin is preferred in hospitals where staphylococci resistant to penicillinase-resistant penicillins frequently cause wound infection and is recommended for patients allergic to penicillins and cephalosporins. For information on current recommendations for perioperative prophylaxis, see Uses: Perioperative Prophylaxis, in the Cephalosporins General Statement 8:12.06.
Dosage and Administration
Administration
Dicloxacillin sodium is administered orally. Nafcillin sodium and oxacillin sodium are administered by IM injection or by slow IV injection or infusion. In general, orally administered penicillinase-resistant penicillins should not be used for the initial treatment of severe infections and should not be relied on in patients with nausea, vomiting, gastric dilation, cardiospasm, or intestinal hypermotility. Since food interferes with GI absorption of penicillinase-resistant penicillins, the drugs should be administered orally at least 1 hour before or 2 hours after meals.
Dosage
Dosage adjustments generally are unnecessary when dicloxacillin, nafcillin, or oxacillin is used in patients with renal impairment; however, some clinicians suggest that the lower range of the usual dosage of oxacillin be used in these patients. Dosage of nafcillin may need to be adjusted if the drug is used in patients with both impaired renal function and impaired hepatic function.
Cautions
As with other penicillins, hypersensitivity reactions are among the most frequent adverse reactions to penicillinase-resistant penicillins. The frequency and severity of adverse effects generally are similar among the penicillinase-resistant penicillins, although hepatotoxicity has been reported most frequently in patients receiving IV oxacillin and adverse renal effects have been reported most frequently in patients receiving IV methicillin (no longer commercially available in the US).
Sensitivity Reactions
Hypersensitivity reactions reported with penicillinase-resistant penicillins are similar to those reported with other penicillins; however, severe hypersensitivity reactions have been reported less frequently with penicillinase-resistant penicillins than with natural penicillins.
Hypersensitivity reactions reported with penicillinase-resistant penicillins include rash (morbilliform, maculopapular, urticarial, or erythematous), fever, eosinophilia, pruritus, and serum sickness-like reactions with fever, chills, and myalgia. Eosinophilia reportedly occurs in 5-38% of patients receiving a penicillinase-resistant penicillin and fever or rash reportedly occurs in 2-6% of patients receiving one of these drugs.
Acute hemolytic anemia has been reported in one patient who received oral dicloxacillin in conjunction with IV nafcillin; however, it is not clear whether this was a hypersensitivity reaction to the drugs since the direct antiglobulin test result in this patient was negative. Anaphylaxis has been reported rarely with penicillinase-resistant penicillins. If a severe hypersensitivity reaction occurs during therapy with a penicillinase-resistant penicillin, the drug should be discontinued and the patient given appropriate treatment (e.g., epinephrine, corticosteroids, maintenance of an adequate airway, oxygen) as indicated.
For a more complete discussion on manifestations of penicillin hypersensitivity and information on the mechanisms of these reactions, the management of patients with hypersensitivity reactions, and how to identify patients at high risk for hypersensitivity reactions to penicillins, see Cautions: Hypersensitivity Reactions, in the Natural Penicillins General Statement 8:12.16.04.
Hematologic Effects
In addition to eosinophilia and hemolytic anemia (see Cautions: Sensitivity Reactions), other adverse hematologic effects including transient neutropenia, leukopenia, granulocytopenia, and thrombocytopenia have occurred rarely with penicillinase-resistant penicillins. Agranulocytosis also has been reported rarely with IV nafcillin and oxacillin. Although adverse hematologic effects have been reported most frequently in patients receiving high dosages of the drugs parenterally, these reactions have occurred following oral administration.
In most reported cases, leukopenia or neutropenia was evident only after 10 or more days of therapy with a penicillinase-resistant penicillin and resolved 2-7 days following discontinuance of the drug. In some cases, leukopenia and neutropenia appeared to be hypersensitivity reactions to the drugs since they had a rapid onset after initiation of therapy (within 48 hours) and recurred with subsequent penicillin therapy. In other reported cases, these adverse hematologic effects appeared to result from a dose-related toxic effect on the bone marrow and did not always recur when therapy was initiated with lower dosages of another penicillin. Prolonged bleeding time, which appeared to result from platelet dysfunction, has been reported rarely with IV nafcillin.
GI Effects
Some of the most frequent adverse reactions to orally administered penicillinase-resistant penicillins are GI effects including nausea, vomiting, epigastric distress, loose stools,diarrhea, and flatulence. These effects rarely are severe enough to require discontinuance of the drugs. Black or hairy tongue and oral lesions including glossitis and stomatitis also have been reported with penicillinase-resistant penicillins.
Clostridium difficile-associated diarrhea and colitis (also known as antibiotic-associated pseudomembranous colitis) has been reported rarely with penicillinase-resistant penicillins; C. difficile has been isolated in feces of several children who developed diarrhea while receiving oral dicloxacillin or oral oxacillin (no longer commercially available in the US) and also has been isolated from patients receiving IV oxacillin. Mild cases of colitis may respond to discontinuance of the penicillinase-resistant penicillin alone, but management of moderate to severe cases should include treatment with fluid, electrolyte, protein supplementation, and appropriate anti-infective therapy (e.g., oral metronidazole, oral vancomycin) as indicated. Administration of oral dicloxacillin has rarely resulted in acute hemorrhagic colitis with severe abdominal pain and GI bleeding, but without evidence of C. difficile-associated diarrhea and colitis.
Renal Effects
Acute Interstitial Nephritis Acute interstitial nephritis, manifested by fever, rash, eosinophilia, macroscopic or microscopic hematuria, azotemia, dysuria, oliguria, proteinuria, pyuria, cylindruria, and eosinophiluria, occurs occasionally with methicillin (no longer commercially available in the US). The onset of symptoms varies from 5 days to 5 weeks after initiation of therapy with the drug; however, renal function can deteriorate rapidly and failure to recognize the condition may lead to progressive renal failure and death.
Although azotemia has been reported to persist for several months in some patients and permanent renal impairment has been reported rarely, interstitial nephritis reported with methicillin therapy generally is reversible following discontinuance of the drug. Interstitial nephritis generally recurs if methicillin is readministered to a patient who developed the adverse effect while receiving the drug previously. In addition, administration of ampicillin, oxacillin, or nafcillin to patients who developed acute interstitial nephritis while receiving methicillin also has resulted in recurrence of the nephritis.
Administration of corticosteroids has been reported to hasten recovery from methicillin-induced interstitial nephritis in some cases; however, there are no controlled studies to date that demonstrate that corticosteroids have an effect on resolution of the nephritis.
Acute interstitial nephritis has been reported more frequently with methicillin than with currently available penicillins. Acute interstitial nephritis has been reported in up to 17% of patients receiving IV methicillin, most frequently in patients receiving prolonged therapy or methicillin dosages of more than 200 mg/kg daily. In one study, hematuria occurred in 4-8% of children receiving IV methicillin in dosages of 170-380 mg/kg daily.
Acute interstitial nephritis also has been reported rarely with IV nafcillin and IV oxacillin. In addition, acute interstitial nephritis has been reported rarely with other penicillins, including penicillin G, amoxicillin, ampicillin, and carbenicillin, Acute interstitial nephritis appears to be a hypersensitivity reaction to penicillins; however, several possible immunologic mechanisms have been identified.
The reaction may be mediated by IgG and IgM antibodies specific for the penicilloyl hapten group of the drugs; the penicilloyl hapten of methicillin appears to bind to renal structural proteins in the tubular basement membrane which may stimulate an immune response to the antigen-protein complex. In addition, circulating antibodies to tubular basement membrane have been detected in a few patients who developed interstitial nephritis during methicillin therapy. Renal biopsy generally indicates severe interstitial disease with edema and a mononuclear cell infiltrate in the tubules; the glomeruli are usually normal.
Other Adverse Renal Effects
Hypokalemia with excessive urinary loss of potassium has been reported rarely in patients receiving nafcillin in dosages of 200-300 mg/kg daily; in several cases, the hypokalemia resolved when dosage of the drug was reduced to 100-150 mg/kg. Although it has been suggested that hypokalemia during penicillin therapy may result from redistribution of potassium within the body, hypokalemia appears to be related to the fact that penicillins act as nonabsorbable anions in the distal renal tubules and therefore promote urinary loss of potassium.
Hepatic Effects
Hepatic dysfunction resembling hepatitis or intrahepatic cholestasis occurs occasionally during therapy with IV oxacillin, especially when high dosage (e.g., 12 g or more daily) is used. Hepatotoxicity is manifested by elevations in serum concentrations of alkaline phosphatase, AST (SGOT), ALT (SGPT), and LDH and may be associated with concomitant fever, anorexia, nausea, vomiting, hepatomegaly, eosinophilia, and rash.If hepatotoxicity occurs during oxacillin therapy, elevations in serum liver enzyme concentrations are generally detectable 2-24 days after initiation of therapy and effects are generally reversible following discontinuance of the drug. In several reported cases, hepatotoxicity resolved and did not recur when therapy was changed to nafcillin. However, elevations in serum aminotransferase concentrations persisted in at least one patient following discontinuance of oxacillin and initiation of nafcillin therapy.
It has been suggested that in most reported cases, hepatic dysfunction during oxacillin therapy was the result of a hypersensitivity reaction to the drug. However, some clinicians suggest that hepatotoxicity may result from a direct, dose-related toxic effect of the drug, since it appears to occur more commonly in patients receiving relatively high dosages of oxacillin.
Limited evidence suggests that patients with human immunodeficiency virus (HIV) infection may be at greater risk of developing hepatoxicity than other patients. Although the clinical importance is unclear, asymptomatic and transient increases in serum concentrations of alkaline phosphatase, AST, and ALT have been reported occasionally with oral dicloxacillin and parenteral therapy nafcillin.
Nervous System Effects
Adverse nervous system effects similar to those reported with penicillin G have been reported rarely with penicillinase-resistant penicillins (e.g., oxacillin), especially when large dosages were administered IV to patients with impaired renal function. Seizures and clonus occurred in one patient with impaired renal function following IV administration of 12 g of oxacillin daily. Neurotoxicity in this patient appeared to be associated with high CSF concentrations of oxacillin since CSF concentrations of the drug were 70 mcg/mL at the time of seizures and 6 mcg/mL 48 hours later when seizures had subsided.
Local Reactions
IV administration of nafcillin or oxacillin occasionally results in phlebitis or thrombophlebitis, especially when the drugs are administered to geriatric patients. Extravasation of nafcillin can cause potentially severe chemical irritation of perivascular tissues, possibly resulting in ulceration, tissue necrosis, sloughing (including full-thickness skin loss), and gangrene; occasionally, surgical debridement and skin grafting have been necessary, including in several infants and children.
To reduce the risk of thrombophlebitis and other local reactions, the manufacturers suggest that IV nafcillin therapy be used only for short periods of time (24-48 hours) whenever possible, and at recommended concentrations. If the patient complains of pain during IV infusion of nafcillin, the infusion should be stopped immediately and the patient evaluated for possible thrombophlebitis or perivascular extravasation. If extravasation is present, some clinicians suggest that local injury can be minimized by prompt infiltration of hyaluronidase at the extravasated site. Sterile abscesses at the injection site have occurred rarely following IM administration of penicillinase-resistant penicillins.
Precautions and Contraindications
Dicloxacillin, nafcillin, and oxacillin are contraindicated in patients who are hypersensitive to any penicillin. Prior to initiation of therapy with a penicillinase-resistant penicillin, careful inquiry should be made concerning previous hypersensitivity reactions to penicillins, cephalosporins, or other drugs. There is clinical and laboratory evidence of partial cross-allergenicity among penicillins and other b-lactam antibiotics including cephalosporins and cephamycins.
Although it has not been proven that allergic reactions to antibiotics are more frequent in atopic individuals, the manufacturers state that penicillinase-resistant penicillins should be used with caution in patients with a history of allergy, particularly to drugs.
For more information on hypersensitivity reactions to penicillins and precautions associated with these reactions, see Cautions: Hypersensitivity Reactions, in the Natural Penicillins General Statement 8:12.16.04.
Renal, hepatic, and hematologic systems should be evaluated periodically during prolonged therapy with a penicillinase-resistant penicillin. Because adverse hematologic effects have occurred during therapy with penicillinase-resistant penicillins (see Cautions: Hematologic Effects), total and differential white blood cell (WBC) counts should be performed prior to initiation of therapy with the drugs and 1-3 times weekly during therapy. Urinalysis should be performed and serum creatinine and BUN concentrations should be determined prior to and periodically during penicillinase-resistant penicillin therapy.
AST (SGOT) and ALT (SGPT) should also be determined periodically during therapy to monitor for hepatotoxicity. Prolonged use of penicillinase-resistant penicillins may result in overgrowth of nonsusceptible organisms, including fungi or gram-negative bacteria such as Pseudomonas. Careful observation of the patient during therapy with a penicillinase-resistant penicillin is essential. If suprainfection or superinfection occurs, the drug should be discontinued and appropriate therapy instituted.
Pediatric Precautions
Penicillinase-resistant penicillins should be used with caution in neonates since elimination of penicillins is delayed in this age group. When penicillinase-resistant penicillins are administered to neonates, serum concentrations of the drugs should be monitored and appropriate reductions in dosage and frequency of administration made when indicated; organ systems should also be evaluated frequently.
Mutagenicity and Carcinogenicity
It is not known if penicillinase-resistant penicillins are mutagenic or carcinogenic in humans.
Pregnancy, Fertitlity and Lactation
Safe use of dicloxacillin, nafcillin, or oxacillin during pregnancy has not been definitely established. Reproduction studies in mice, rats, and rabbits using penicillinase-resistant penicillins have not revealed evidence of impaired fertility or harm to the fetus. Clinical experience with use of penicillins during pregnancy in humans has not revealed evidence of adverse effects on the fetus. However, there are no adequate and controlled studies in pregnant women, and penicillinase-resistant penicillins should be used during pregnancy only when clearly needed. Because dicloxacillin and oxacillin are distributed into milk, penicillinase-resistant penicillins should be used with caution in nursing women.
Drug Interactions
For further information on these and other drug interactions reported with penicillins, see Drug Interactions in the Natural Penicillins General Statement 8:12.16.04. Although not all drug interactions reported with other penicillins have been reported with penicillinase-resistant penicillins, the fact that some of these interactions could occur with the drugs should be considered.
Aminoglycosides
Synergism with Aminoglycosides In vitro studies indicate that a synergistic bactericidal effect can occur against penicillinase-producing and nonpenicillinase-producing S. aureus susceptible to penicillinase-resistant penicillins when nafcillin or oxacillin is used in conjunction with an aminoglycoside (e.g., gentamicin, tobramycin). Although the clinical importance is unclear, in vitro synergism has also been reported against some strains of oxacillin-resistant S. aureus (previously known as methicillin-resistant S. aureus) when high concentrations of nafcillin or oxacillin were used in conjunction with amikacin, gentamicin, or kanamycin.
Incompatibility with Aminoglycosides
Penicillinase-resistant penicillins, like other penicillins, are physically and/or chemically incompatible with aminoglycosides and can inactivate the drugs in vitro. If concomitant therapy is indicated, in vitro mixing of penicillinase-resistant penicillins and aminoglycosides should be avoided and the drugs should be administered separately. Penicillinase-resistant penicillins can also inactivate aminoglycosides in vitro in serum samples obtained from patients receiving concomitant therapy with the drugs. This could adversely affect results of serum aminoglycoside assays performed on the serum samples. (See Laboratory Test Interferences: Serum Aminoglycoside Assays.)
Cyclosporine
Concomitant administration of nafcillin and cyclosporine can result in decreased cyclosporine concentrations. In one patient receiving cyclosporine concomitantly with nafcillin, serum concentrations of cyclosporine decreased to subtherapeutic levels during 2 separate courses of therapy. It has been suggested that nafcillin may increase hepatic metabolism of cyclosporine probably by induction of hepatic microsomal enzymes resulting in decreased serum concentrations of cyclosporine. The manufacturer of nafcillin suggests that cyclosporine concentrations should be monitored if nafcillin is used concomitantly. Some clinicians suggest that an alternative anti-infective be used in patients receiving cyclosporine.
Probenecid
Oral probenecid administered shortly before or simultaneously with penicillinase-resistant penicillins slows the rate of renal tubular secretion of the penicillins and produces higher and prolonged serum concentrations of the drugs. In one study, probenecid decreased the volume of distribution of nafcillin by about 20%.
Rifampin
In vitro studies indicate that antagonism can occur when nafcillin or oxacillin is used in conjunction with rifampin against S. aureus. However, antagonism between the drugs appears to be dose-dependent and occurs only when high concentrations of the penicillin are present. In vitro studies indicate that when low concentrations of oxacillin are present, indifference or synergism generally occurs. Although some clinicians suggest that rifampin not be used concomitantly with penicillins, concomitant use of oxacillin and rifampin appears to delay or prevent the emergence of rifampin-resistant strains of S. aureus and the drugs have been used concomitantly with no apparent decrease in activity.
Tetracyclines
Tetracyclines may antagonize the bactericidal effects of penicillins, including penicillinase-resistant penicillins, and concomitant administration of the drugs should be avoided.
Warfarin
Concomitant administration of nafcillin or dicloxacillin and warfarin has been reported to decrease the hypoprothrombinemic effect of the anticoagulant. In several patients (some of whom were stabilized on warfarin), IV nafcillin (usually given in high dosages of 9-12 g daily) decreased the hypoprothrombinemic effect of the anticoagulant. It has been suggested that nafcillin may decrease the serum half-life of warfarin by increasing metabolism of the anticoagulant, probably by induction of hepatic microsomal enzymes.
Prothrombin time should be monitored carefully during concomitant administration of a penicillinase-resistant penicillin and a coumarin anticoagulant and for several weeks after discontinuance of the penicillin, since in some patients prothrombin time did not return to pretreatment levels until about 30 days after discontinuance of nafcillin. Dosage of the anticoagulant should be adjusted as required when a penicillinase-resistant penicillin is administered to a patient receiving a coumarin anticoagulant.
Laboratory Test Interferences
For more complete information on these and other laboratory test interferences reported with penicillins, see Laboratory Test Interferences in the Natural Penicillins General Statement 8:12.16.04. Although not all laboratory test interferences reported with other penicillins have been reported with penicillinase-resistant penicillins, the possibility that these interferences could occur with the drugs should be considered.
Tests for Urinary and Serum Proteins
Like other penicillins, penicillinase-resistant penicillins interfere with or cause false-positive results in a variety of test methods used to determine urinary or serum proteins. Studies using oxacillin and nafcillin indicate that the drugs cause false-positive or falsely elevated results in turbidimetric methods for urinary and serum proteins that use sulfosalicylic acid or trichloroacetic acid. Nafcillin also interferes with tests for urinary protein that use the biuret reagent and can cause slightly increased urinary protein concentrations when the Coomassie brilliant blue method is used. Nafcillin does not appear to interfere with tests for urinary protein that use bromphenol-blue (Albustix®, Albutest®).
Serum Aminoglycoside Assays
Because penicillinase-resistant penicillins inactivate aminoglycosides in vitro (see Drug Interactions: Aminoglycosides), presence of the drugs in serum samples to be assayed for aminoglycoside concentrations may result in falsely decreased results. For more information on this laboratory test interference, see Laboratory Test Interferences: Serum Aminoglycoside Assays, in the Natural Penicillins General Statement 8:12.16.04.
Mechanism of Action
Penicillinase-resistant penicillins have a mechanism of action similar to that of other penicillins. For information on the mechanism of action of penicillins, see Mechanism of Action in the Natural Penicillins General Statement 8:12.16.04. Spectrum The commercially available penicillinase-resistant penicillins (dicloxacillin, nafcillin, oxacillin) have similar spectra of activity. Penicillinase-resistant penicillins are active in vitro against many gram-positive aerobic cocci. Because penicillinase-resistant penicillins are not inactivated by most staphylococcal penicillinases, the drugs are active against many penicillinase-producing strains of Staphylococcus aureus and S. epidermidis that are resistant to other commercially available penicillins. Penicillinase-resistant penicillins also are active in vitro against a few gram-positive aerobic and anaerobic bacilli and some gram-negative cocci; however, the drugs generally are inactive against gram-negative aerobic and anaerobic bacilli. Penicillinase-resistant penicillins are inactive against mycobacteria, Mycoplasma, Rickettsia, fungi, and viruses.
In Vitro Susceptibility Testing
Results of in vitro susceptibility tests with penicillinase-resistant penicillins may be affected by inoculum size, period of incubation, pH of the media, or the presence of human serum.
Detection of oxacillin-resistant staphylococci (ORSA; previously known as methicillin-resistant staphylococci or MRSA) generally requires use of specialized testing procedures and culture media. In vitro, the expression of resistance to penicillinase-resistant penicillins is influenced by temperature, pH, and sodium chloride concentration of the media. To optimize detection of oxacillin-resistant staphylococci in dilution susceptibility testing, the National Committee for Clinical Laboratory Standards (NCCLS) recommends addition of 2% sodium chloride to the broth or agar dilution media, use of the direct method of colony suspension (equivalent to a 0.5 McFarland standard), and incubation for 24 hours at 35°C. NCCLS states that oxacillin is the preferred derivative for in vitro testing since the drug is more resistant to degradation during storage than other penicillinase-resistant penicillins and more likely to detect heteroresistant staphylococci.
Standard in vitro susceptibility tests cannot detect tolerance to penicillinase-resistant penicillins because the minimum inhibitory concentrations (MICs) of tolerant and nontolerant strains are generally similar and these tests do not directly measure bactericidal activity. This fact should be considered when evaluating results of in vitro susceptibility tests. For information on tolerance, see Resistance: Tolerance.
Disk Diffusion Tests
When the disk-diffusion procedure is used to test in vitro susceptibility to penicillinase-resistant penicillins, a disk containing 1 mcg of oxacillin may be used and results can be applied to all currently available penicillinase-resistant penicillins (dicloxacillin, nafcillin, oxacillin). NCCLS states that an oxacillin disk is preferred since it is more resistant to degradation in storage and because it is more likely to detect heteroresistant staphylococci. Although a disk containing 1 mcg of nafcillin may be used to determine susceptibility of S. aureus, interpretive criteria have not been established for testing other staphylococci using a nafcillin disk.
When disk-diffusion susceptibility testing is performed according to NCCLS standardized procedures using the 1-mcg oxacillin disk or the 1-mcg nafcillin disk, S. aureus with growth inhibition zones of 13 mm or greater are susceptible to penicillinase-resistant penicillins, those with zones of 11-12 mm have intermediate susceptibility, and those with zones of 10 mm or less are resistant to the drugs. S. aureus with intermediate susceptibility to penicillinase-resistant penicillins should be tested further using the oxacillin-salt agar screening test.
When the disk-diffusion procedure is performed according to NCCLS standardized procedures using the 1-mcg oxacillin disk, coagulase-negative staphylococci with growth inhibition zones of 18 mm or greater are susceptible to penicillinase-resistant penicillins and those with zones of 17 mm or less are resistant to the drugs. Interpretive criteria for coagulase-negative staphylococci correlate with the presence or absence of the mecA gene that encodes resistance to penicillinase-resistant penicillins in S. epidermidis. These criteria may overcall resistance for other coagulase-negative staphylococci (e.g., S. lugdunensis, S. saprophyticus).
For serious infections with coagulase-negative staphylococci other than S. epidermidis, testing for mecA or the protein expressed by mecA (penicillin-binding protein 2a [PBP 2a]) may be appropriate for strains having zone diameters in the intermediate or resistant range. Isolates that are shown to carry mecA or produce PBP 2a should be reported as oxacillin resistant.
Dilution Susceptibility Tests
When dilution susceptibility testing (agar or broth dilution) is performed according to NCCLS standardized procedures using oxacillin or nafcillin, S. aureus with MICs of 2 mcg/mL or less are susceptible to penicillinase-resistant penicillins and those with MICs of 4 mcg/mL or greater are resistant to the drugs. When dilution susceptibility testing is performed according to NCCLS standardized procedures using oxacillin, coagulase-negative staphylococci with MICs of 0.25 mcg/mL or less are susceptible to penicillinase-resistant penicillins and those with MICS of 0.5 mcg/mL or greater are resistant to the drugs. Interpretive criteria for coagulase-negative staphylococci correlate with the presence or absence of the mecA gene that encodes resistance to penicillinase-resistant penicillins in S. epidermidis.
These criteria may overcall resistance for other coagulase-negative staphylococci (e.g., S. lugdunensis, S. saprophyticus). For serious infections with coagulase-negative staphylococci other than S. epidermidis, testing for mecA or PBP 2a may be appropriate for strains having MICs of 0.5-2 mcg/mL. Staphylococcal isolates that are shown to carry mecA or that produce PBP 2a should be reported as oxacillin resistant.
Gram-Positive Aerobic Bacteria
Gram-Positive Aerobic Cocci Penicillinase-resistant penicillins are active in vitro against many gram-positive aerobic cocci including penicillinase-producing and nonpenicillinase-producing strains of S. aureus and S. epidermidis. In addition to S. epidermidis, the drugs are active in vitro against some other coagulase-negative staphylococci including some strains of S. haemolyticus, S. hominis, S. lugdunensis, S. saprophyticus S. schleiferi, S. simulans, and S. warneri. However, many strains of coagulase-negative staphylococci are resistant to penicillinase-resistant penicillins.
Penicillinase-resistant penicillins are active in vitro against Streptococcus pyogenes (group A b-hemolytic streptococci), S. agalactiae (group B streptococci), groups C and G streptococci, S. pneumoniae, and some viridans streptococci. Enterococci, including E. faecalis (formerly S. faecalis), usually are resistant to the drugs. Nonpenicillinase-producing strains of S. aureus usually are inhibited in vitro by dicloxacillin, nafcillin, or oxacillin concentrations of 0.1-0.8 mcg/mL and penicillinase-producing strains of S. aureus usually are inhibited by concentrations of 0.3-1.6 mcg/mL.
Susceptible strains of S. epidermidis usually are inhibited by oxacillin concentrations of 0.125 mcg/mL or less. With the exception of penicillinase-producing staphylococci, penicillinase-resistant penicillins generally are less active in vitro on a weight basis than natural penicillins against susceptible gram-positive cocci. The MIC90 (minimum inhibitory concentration of the drug at which 90% of strains tested are inhibited) of dicloxacillin, nafcillin, or oxacillin reported for most susceptible S. pneumoniae and groups A, B, C, and G streptococci is 0.1-0. mcg/mL. Viridans streptococci generally are inhibited in vitro by penicillinase-resistant penicillin concentrations of 0.1-1.6 mcg/mL.
Gram-Positive Aerobic Bacilli
Penicillinase-resistant penicillins are active in vitro against a few gram-positive aerobic bacilli. Corynebacterium diphtheriae reportedly is inhibited in vitro by oxacillin concentrations of 1.6-3.1 mcg/mL. In vitro, oxacillin concentrations of 0.01-0.03 mcg/mL inhibit some strains of Erysipelothrix rhusiopathiae.
Gram-Negative Aerobic Bacteria
Neisseria
Although penicillinase-resistant penicillins generally are less active in vitro on a weight basis than natural penicillins against gram-negative aerobic cocci, the drugs are active in vitro against some strains of Neisseria meningitidis and N. gonorrhoeae. N. meningitidis generally requires dicloxacillin, nafcillin, or oxacillin concentrations of 0.5-8 mcg/mL for in vitro inhibition. Penicillinase-producing and nonpenicillinase-producing strains of N. gonorrhoeae generally are inhibited in vitro by penicillinase-resistant penicillin concentrations of 1.6-12.5 mcg/mL.
Haemophilus
Some strains of Haemophilus influenzae reportedly are inhibited in vitro by nafcillin concentrations of 1-12. mcg/mL; however, most strains of the organism are resistant to penicillinase-resistant penicillins.
Other Gram-Negative Aerobes
Pasteurella multocida, an organism that can be aerobic or facultatively anaerobic, reportedly is inhibited in vitro by dicloxacillin, nafcillin, or oxacillin concentrations of 3.1-12.5 mcg/mL. Penicillinase-resistant penicillins generally are inactive against other gram-negative aerobic bacilli including Enterobacteriaceae and Pseudomonas.
Anaerobic Bacteria
Some gram-positive anaerobic bacteria, including some strains of Actinomyces, Clostridium, Peptococcus, and Peptostreptococcus, are inhibited in vitro by penicillinase-resistant penicillins; however, penicillinase-resistant penicillins are less active against these organisms than other penicillins. Gram-negative anaerobic bacteria, including Bacteroides, generally are resistant to penicillinase-resistant penicillins.
Spirochetes
Penicillinase-resistant penicillins have some activity against spirochetes, although less than that of the natural penicillins. Resistance For a discussion of the possible mechanisms of bacterial resistance to penicillins, see Resistance: Mechanisms of Penicillin Resistance in the Natural Penicillins General Statement 8:12.16.04. Complete cross-resistance generally occurs among penicillinase-resistant penicillins. Minor differences in the degree of resistance to the various penicillinase-resistant penicillins have been reported in results of in vitro susceptibility tests; however, resistance to any penicillinase-resistant penicillin should be interpreted as resistance to all currently available penicillinase-resistant penicillins.
Oxacillin-Resistant Staphylococci
Although in the past both penicillinase-producing and nonpenicillinase-producing staphylococci generally were susceptible to penicillinase-resistant penicillins, staphylococci resistant to penicillinase-resistant penicillins have been reported with increasing frequency. Historically, staphylococci resistant to penicillinase-resistant penicillins have been referred to as methicillin-resistant staphylococci and methicillin-resistant Staphylococcus aureus have been referred to as MRSA; however, methicillin is no longer commercially available in the US and oxacillin has become the preferred drug for testing in vitro susceptibility to penicillinase-resistant penicillins.
Therefore, although the prior terminology may still be used, staphylococci resistant to penicillinase-resistant penicillins are now being referred to as oxacillin-resistant staphylococci and oxacillin-resistant S. aureus are being referred to as ORSA. In the US, up to 50% of clinical isolates of S. aureus and up to 80% of clinical isolates of coagulase-negative staphylococci are oxacillin-resistant. Approximately 63-79% of S. epidermidis isolates from patients with prosthetic valve endocarditis or infected CNS shunts reportedly are oxacillin-resistant.
Data obtained from some US hospitals between 1998-1999 indicated that about 35% of clinical isolates of S. aureus from hospitalized patients and about 23% from outpatients were oxacillin-resistant strains and 64-74% of coagulase-negative staphylococci from hospitalized patients and about 44% from outpatients were oxacillin-resistant strains. Surveillance data from 33 US hospitals during 2000 indicate that 45.% of S. aureus isolates obtained from hospitalized patients and 28.% of isolates obtained from outpatients were resistant to penicillinase-resistant penicillins. Resistance to penicillinase-resistant penicillins is intrinsic and usually is mediated by the presence of the mecA gene that encodes a specific penicillin-binding protein (PBP 2a) that has a low affinity for and is not inhibited by b-lactam antibiotics.
Resistant to penicillinase-resistant penicillins may also occur as the result of penicillinase production or modification of existing PBPs. Isolates of oxacillin-resistant staphylococci, especially coagulase-negative staphylococci, generally are heterogeneous and only a small portion of the cells may demonstrate resistance in vitro. Therefore detection of oxacillin resistance is complex and resistant isolates may not always be detected by routine in vitro susceptibility testing. (See Spectrum: In Vitro Susceptibility Testing.) In addition to being cross-resistant to all currently available penicillins, oxacillin-resistant staphylococci generally are resistant to other b-lactam antibiotics including first, second, or third generation cephalosporins. These strains also generally are resistant to tetracyclines, chloramphenicol, macrolides, and clindamycin and may be resistant to aminoglycosides and fluoroquinolones. However, most strains of oxacillin-resistant staphylococci are susceptible to vancomycin or co-trimoxazole and may be susceptible to rifampin.
Tolerance
Tolerance to the bactericidal effects of penicillinase-resistant penicillins has been reported in 30-63% of clinical isolates of S. aureus. Tolerance to the bactericidal effects of oxacillin has also been reported rarely in S. epidermidis.
Most staphylococci susceptible to penicillinase-resistant penicillins have an MBC (minimum bactericidal concentration) of the drugs that is 1-4 times greater than the MIC of the drugs; however, bacteria with an MBC that is 16 or more times greater than the MIC of the drugs are generally considered tolerant to penicillinase-resistant penicillins. Results of some studies indicate that all isolates of S. aureus contain a small percentage of tolerant strains and that high MBCs are only detectable when a substantial percentage of tolerant organisms is present. The clinical importance of tolerance has not been fully elucidated.
In vitro, bacteria tolerant to penicillinase-resistant penicillins may be inhibited by the drugs but are either not killed or are killed at a slower rate than bacteria that are not tolerant. Infections caused by tolerant bacteria may persist during therapy although in vitro susceptibility tests indicate that the organisms are susceptible to the drugs. The presence of tolerant staphylococci in serious infections where rapid and complete bactericidal activity is important (e.g., endocarditis, bacteremia) could result in a less favorable response to penicillinase-resistant penicillin therapy.
Therefore, although the value of concomitant therapy has not been definitely established, some clinicians suggest that a rapidly bactericidal anti-infective (e.g., an aminoglycoside) be used in conjunction with a penicillinase-resistant penicillin for the treatment of severe infections caused by tolerant staphylococci. (See Penicillin-Tolerant Staphylococcal Infections in Uses: Staphylococcal Infections.) Tolerance appears to occur in strains that have a deficiency in an autolytic enzyme on their cell surface that is necessary for the bactericidal effect of penicillins or may be the result of the presence of an autolysin inhibitor. Staphylococci that are tolerant to penicillinase-resistant penicillins may also be cross-tolerant to some cephalosporins and/or vancomycin.
Resistance in Gram-Negative Bacteria
Gram-negative bacteria generally are intrinsically resistant to penicillinase-resistant penicillins because the bulky side chains of the drugs, which help to protect these derivatives from hydrolysis by penicillinases, also prevent the drugs from penetrating the outer membrane of most gram-negative bacteria.
Pharmacokinetics
For more specific information on the pharmacokinetics of dicloxacillin, nafcillin, and oxacillin, see Pharmacokinetics in the individual monographs in 8:12.16.12. In all studies described in the pharmacokinetics section, penicillinase-resistant penicillins were administered as sodium salts. Dosages and concentrations of dicloxacillin sodium, nafcillin sodium, and oxacillin sodium are expressed in terms of their bases.
Absorption
Like other penicillins, absorption of orally administered penicillinase-resistant penicillins occurs mainly in the duodenum and upper jejunum and the rate and extent of absorption depend on the particular penicillin derivative, dosage form administered, gastric and intestinal pH, and presence of food in the GI tract. Isoxazolyl penicillins (cloxacillin [no longer commercially available in the US], dicloxacillin, oxacillin) are acid stable and are rapidly but incompletely absorbed from the GI tract.
In healthy, fasting adults, approximately 35-76% of an orally administered dose of dicloxacillin or 30-35% of an orally administered dose of oxacillin (oral dosage forms no longer commercially available in the US) is absorbed from the GI tract. Following oral administration of a single oral dose of dicloxacillin or oxacillin in healthy, fasting adults, peak serum concentrations of the drugs usually are attained within 30 minutes to 2 hours; serum concentrations of the drugs then decline rapidly and generally are low or undetectable 4-6 hours after the dose. In one study in healthy, fasting adults, oral administration of a single 500-mg dose of dicloxacillin or oxacillin as capsules resulted in peak serum concentrations of the drugs ranging from 5-7 mcg/mL, 7.5-14.4 mcg/mL, or 10-17 mcg/mL, respectively.
Presence of food in the GI tract generally decreases the rate and extent of absorption of penicillinase-resistant penicillins. Oxacillin is rapidly absorbed from IM injection sites. Following IM administration of single 1-g doses of oxacillin in adults, peak serum concentrations of the drug range from 6-18 mcg/mL and generally are attained within 30-60 minutes; serum concentrations then decline rapidly and are low or undetectable 4-6 hours after the dose. Rapid IV injection of a single 500-mg or 1-g dose of nafcillin or oxacillin generally results in peak serum concentrations of the drugs that range from 26-63 mcg/mL immediately following injection; however, serum concentrations of the drugs are low or undetectable 2-3 hours later.
Distribution
Penicillinase-resistant penicillins are widely distributed following absorption from the GI tract or injection sites. The volume of distribution of oxacillin reportedly is 0.39-0.43 L/kg in healthy adults. The volume of distribution of nafcillin reportedly ranges from 0.57-1.55 L/kg in adults, 0.85-0.91 L/kg in children 1 month to 14 years of age, and 0.24-0.53 L/kg in neonates.
Nafcillin has a greater volume of distribution than other currently available penicillins, presumably because it is sequestered in the liver. Concomitant administration of oral probenecid may decrease the volume of distribution of nafcillin. (See Drug Interactions: Probenecid.) Penicillinase-resistant penicillins are readily distributed into ascitic, synovial, pleural, and pericardial fluids. The drugs also are distributed into kidneys, liver, gallbladder, bone, bile, skin, intestines, prostate, tonsils, and muscle. Unlike natural penicillins, therapeutic concentrations of penicillinase-resistant penicillins may be attained in bone following parenteral administration of the drugs.
Following IM or IV administration of oxacillin, bone concentrations of the drug reportedly may be 5-23% of concurrent serum concentrations. Penicillinase-resistant penicillins are distributed into bile in varying degrees. Small amounts of isoxazolyl penicillins are distributed into bile; however, concentrations of nafcillin in bile generally are equal to or greater than concurrent serum concentrations of the drugs. Biliary concentrations of the drugs are proportional to hepatobiliary function and may be negligible if biliary obstruction is present. Only negligible concentrations of nafcillin or oxacillin are attained in aqueous humor following oral, IM, or IV administration.
Like natural penicillins, only minimal concentrations of penicillinase-resistant penicillins are attained in CSF following oral, IM, or IV administration in patients with uninflamed meninges. Slightly higher concentrations of the drugs are attained in CSF in patients with inflamed meninges. In one study in patients receiving nafcillin doses of 95-200 mg/kg every 4-6 hours, CSF concentrations of nafcillin were 1.9-30% of concurrent serum concentrations in specimens obtained 1-2 hours after administration of the drug. In one study in rabbits with meningitis, CSF concentrations of nafcillin or oxacillin averaged 1.4-2% or 1-2.8%, respectively, of concurrent serum concentrations of the drugs.
The degree of protein binding varies among penicillinase-resistant penicillins; protein binding of the isoxazolyl penicillins increases with the number of chlorine atoms present on the heterocyclic side chains of the drugs. Dicloxacillin is 95-99%, nafcillin is 70-90%, and oxacillin is 89-94% bound to serum proteins. The drugs bind mainly to serum albumin. All currently available penicillinase-resistant penicillins readily cross the placenta.
The drugs distribute into amniotic fluid. Fetal serum concentrations of oxacillin or dicloxacillin reportedly range from 0-26% of concurrent maternal serum concentrations. Dicloxacillin and oxacillin are distributed into milk. Although specific information on the distribution of nafcillin into milk is not available, this penicillinase-resistant penicillin is probably also distributed into milk.
Elimination
In adults with normal renal function, serum half-lives of dicloxacillin and oxacillin are similar and range from 0.3-0.9 hours. Nafcillin has a slightly longer serum half-life than other penicillinase-resistant penicillins and the serum half-life of the drug in adults with normal renal and hepatic function ranges from 0.5-1.5 hours. The penicillinase-resistant penicillins are metabolized to varying degrees; nafcillin is the most extensively metabolized. Penicillinase-resistant penicillins are partially metabolized by hydrolysis of the b-lactam ring to penicilloic acids which are microbiologically inactive.
Although it has been suggested that following oral administration this hydrolysis occurs partly in the GI tract prior to absorption, the drugs appear to undergo metabolism mainly in the liver following oral or parenteral administration. The extent of inactivation of isoxazolyl penicillins decreases with halogen substitution, and oxacillin is metabolized to a greater extent than is dicloxacillin. In one study following oral administration of single 500-mg oral doses of the drugs, 49% of oxacillin absorbed from the GI tract (oral dosage forms no longer commercially available in the US) was hydrolyzed to penicilloic acids whereas only 10% of dicloxacillin absorbed were hydrolyzed to penicilloic acids. In this study, there was no evidence of 6-APA in urine following oral administration of oxacillin. Isoxazolyl penicillins also appear to be hydroxylated to a small extent to microbiologically active metabolites which are excreted in urine.
The hydroxyl metabolite of dicloxacillin and oxacillin are slightly less active than the parent drugs. Isoxazolyl penicillins and their metabolites are rapidly excreted in urine mainly by tubular secretion and glomerular filtration. These drugs also are partly excreted in feces via biliary elimination. Although small amounts of nafcillin are excreted in urine, the drug is eliminated mainly via bile and undergoes enterohepatic circulation.
Following oral administration of a single 500-mg dose of the drugs in adults with normal renal function, 33-49% of the dicloxacillin dose or 17-70% of the oxacillin dose is excreted in urine as unchanged drug and active metabolites within 6 hours. Only about 27-31% of a single IM or IV dose of nafcillin is excreted in urine as unchanged drug and active metabolites within 12 hours. Approximately 40-70% of a single IM dose of oxacillin is excreted in urine within 6 hours as unchanged drug and active metabolites. Serum clearance of oxacillin in adults with normal renal function has been reported to be 380 mL/minute per 1.73 m. Nafcillin has a serum clearance of 410-583 mL/minute per 1.73 m in adults with normal renal and hepatic function.
Unlike most other penicillins, the serum half-lives of nafcillin, dicloxacillin, and oxacillinare only slightly prolonged in patients with renal impairment. This presumably results from the fact that nafcillin is excreted mainly by nonrenal mechanisms and isoxazolyl penicillins undergo extensive biotransformation to inactive metabolites. The serum half-lives of nafcillin and the isoxazolyl penicillins in patients with renal impairment reportedly range from 0.5-2.8 hours. In one study in patients with cirrhosis, the t1/2a of nafcillin averaged 0.26 hours, the t1/2b of the drug averaged 1.2 hours, and serum clearance of the drug averaged 291.5 mL/minute. Serum concentrations of nafcillin and isoxazolyl penicillins generally are higher and the serum half-lives more prolonged in neonates than in older children.
The serum half-lives of the drugs generally are inversely proportional to birthweight, gestational age, and chronologic age. This appears to result partly from immature mechanisms for conjugation of the drugs in the liver and immature mechanisms for renal tubular secretion. The serum half-life of oxacillin is 1.6 hours in neonates 8-15 days of age and 1.2 hours in neonates 20-21 days of age. In one study, the serum half-life of nafcillin ranged from 2.2-5.5 hours in neonates 3 weeks of age or younger and 1.2-2.3 hours in neonates 4-9 weeks of age.
Oral probenecid administered shortly before or with penicillinase-resistant penicillins competitively inhibits renal tubular secretion of the penicillins and produces higher and prolonged serum concentrations of the drugs. (See Drug Interactions: Probenecid.) Studies using dicloxacillin indicate that patients with cystic fibrosis eliminate the drug up to 3 times faster than healthy individuals because of increased tubular secretion. This effect may be clinically important since use of usual dosages of penicillinase-resistant penicillins in cystic fibrosis patients may result in lower serum concentrations of the drugs than expected. Dicloxacillin, nafcillin, and oxacillin are only minimally removed by hemodialysis or peritoneal dialysis.
Chemistry and Stability
Chemistry
Penicillinase-resistant penicillins are semisynthetic penicillin derivatives produced by acylation of 6-aminopenicillanic acid (6-APA). Penicillinase-resistant penicillins have bulky side chains at R on the penicillin nucleus that result in steric hindrance around the a-carbon of the acylamino group and help to prevent attachment of staphylococcal penicillinases to the b-lactam ring. (For information on the penicillin nucleus, see the Preface to the General Statements on Penicillins 8:12.16.) Penicillinase-resistant penicillins commercially available in the US include dicloxacillin, nafcillin, and oxacillin. Nafcillin is a naphthyl analog of methicillin (no longer commercially available in the US) and has slightly increased acid stability and antibacterial activity compared with methicillin.
Dicloxacillin, oxacillin, and cloxacillin (no longer commercially available in the US) are isoxazolyl penicillins; these penicillinase-resistant penicillins have heterocyclic side chains that result in slightly greater acid stability compared with nafcillin. Oxacillin, cloxacillin, and dicloxacillin differ structurally only in the presence of 0, 1, and 2 chlorine atoms, respectively. The addition of chlorine generally increases in vitro antibacterial activity on a weight basis and increases absorption from the GI tract, serum half-life, and protein binding. Penicillinase-resistant penicillins are commercially available as sodium salts. Potency of the drugs generally is expressed in terms of the bases. In general, penicillinase-resistant penicillins occur as white to off-white crystalline powders and are freely soluble in water and soluble in alcohol.
Stability
Penicillinase-resistant penicillins generally are stable in the dry state at room temperature for several years; however, the drugs are stable only for short periods of time in solution unless frozen. Stability of the drugs is pH and temperature dependent. Nafcillin and oxacillin generally are stable at pH 5-8. Other penicillinase-resistant penicillins are more resistant than nafcillin and oxacillin to acid-catalyzed hydrolysis and generally are stable in the presence of acidic gastric secretions following oral administration. Nafcillin and oxacillin are potentially physically and/or chemically incompatible with some drugs, including aminoglycosides, but the compatibility depends on the specific drug and several other factors (e.g., concentration of the drugs, specific diluents used, resulting pH, temperature). Oxacillin is especially susceptible to inactivation in solutions containing dextrose, which appears to have a catalytic effect on hydrolysis of the drug.
For a more complete discussion of the stability of dicloxacillin, nafcillin, and oxacillin and solutions of the drugs, see Chemistry and Stability: Stability in the individual monographs in 8:12.16.12. For specific information on dosage and administration and additional information on chemistry and stability and pharmacokinetics, see the individual monographs on Dicloxacillin Sodium, Nafcillin Sodium, and Oxacillin Sodium in 8:12.16.12.




