Carbenicillin Indanyl Sodium, Piperacillin Sodium and Tazobactam Sodium, Ticarcillin Disodium, Ticarcillin Disodium and Clavulanate Potassium, Preface to the General Statements on Penicillins
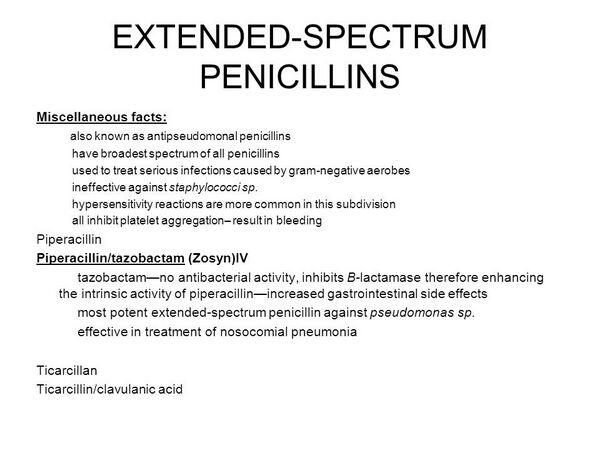
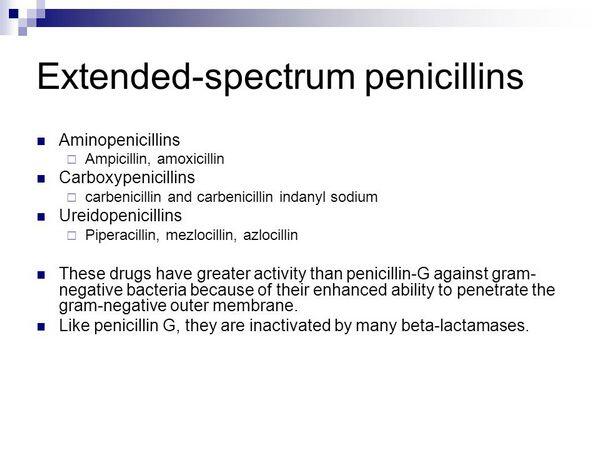
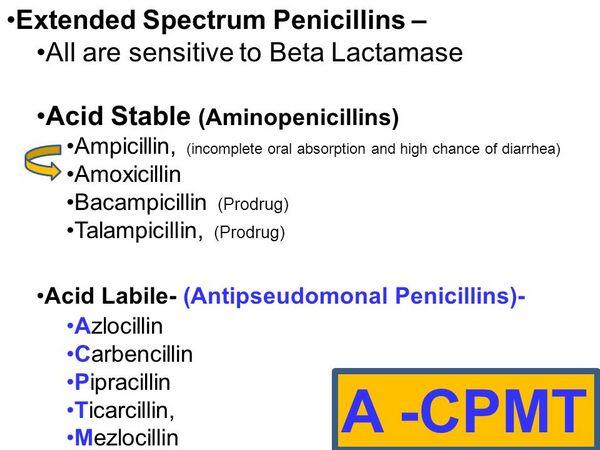
Extended-spectrum penicillins are a group of semisynthetic penicillin antibiotics that, because of their chemical structures, have wider spectra of activity than natural penicillins, penicillinase-resistant penicillins, and aminopenicillins.
Uses
Oral carbenicillin indanyl sodium is used only for the treatment of acute or chronic infections of the upper and lower urinary tract, asymptomatic bacteriuria, or prostatitis caused by susceptible organisms.
Ticarcillin and ticarcillin disodium and clavulanate potassium are used parenterally for the treatment of serious intra-abdominal infections, urinary tract infections, gynecologic infections, respiratory tract infections, skin and skin structure infections, and septicemia caused by susceptible organisms; ticarcillin disodium and clavulanate potassium also is used for the treatment of bone and joint infections caused by susceptible organisms.
Piperacillin sodium and tazobactam sodium is used parenterally for the treatment of intra-abdominal infections, gynecologic infections, skin and skin structure infections, certain respiratory tract infections, and septicemia caused by susceptible organisms.
For further information on the uses of ticarcillin in fixed-ratio combination with clavulanic acid or piperacillin sodium in fixed combination with tazobactam sodium, see Ticarcillin Disodium and Clavulanate Potassium or Piperacillin Sodium and Tazobactam Sodium, respectively, 8:12.16.16. Extended-spectrum penicillins are used principally for the treatment of infections caused by susceptible gram-negative aerobic bacilli and for the treatment of mixed aerobic-anaerobic bacterial infections.
Extended-spectrum penicillins generally should not be used for the treatment of infections, especially infections caused by gram-positive bacteria, when a natural penicillin or an aminopenicillin would be effective. Prior to initiation of therapy with an extended-spectrum penicillin, appropriate specimens should be obtained for identification of the causative organism and in vitro susceptibility tests.
Therapy with an extended-spectrum penicillin may be started pending results of susceptibility tests but should be discontinued if the causative organism is found to be resistant to the drug. Because resistant strains of some organisms, especially Ps. aeruginosa, have developed during therapy with extended-spectrum penicillins, appropriate specimens should be obtained periodically during therapy with the drugs to monitor effectiveness and detect emergence of resistant organisms. In certain severe infections (e.g., sepsis) when the causative organism is unknown or Ps. aeruginosa is suspected, concomitant therapy with an aminoglycoside or third generation cephalosporin should be used initially pending results of in vitro susceptibility tests.
Extended-spectrum penicillins frequently are used in conjunction with aminoglycosides for the treatment of serious infections, especially Ps. aeruginosa infections in patients with cystic fibrosis, or in conjunction with aminoglycosides or third generation cephalosporins for empiric anti-infective therapy in adults with life-threatening sepsis or in febrile granulocytopenic patients. Whenever an aminoglycoside is administered in conjunction with an extended-spectrum penicillin, in vitro mixing of the drugs in syringes or IV infusion containers should be avoided since in vitro studies indicate that b-lactam antibiotics, including extended-spectrum penicillins, may inactivate aminoglycosides. In addition, because in vivo inactivation of aminoglycosides by extended-spectrum penicillins may also occur, some clinicians suggest that it may be advisable to monitor serum aminoglycoside concentrations more closely than usual in patients receiving concomitant therapy, especially when high doses of the extended-spectrum penicillin are administered or when the patient has impaired renal function. (See Drug Interactions: Aminoglycosides.)
Gram-positive Aerobic Bacterial Infections
Extended-spectrum penicillins generally should not be used for the treatment of infections caused by gram-positive aerobic bacteria since the drugs usually are less active in vitro against gram-positive bacteria than natural penicillins or aminopenicillins and have wider spectra of activity than these penicillins. Although extended-spectrum penicillins have been effective when used in the treatment of intra-abdominal infections, urinary tract infections, respiratory tract infections, and gynecologic infections caused by susceptible gram-positive aerobic cocci (e.g., S. pneumoniae, group A b-hemolytic streptococci, nonpenicillinase-producing staphylococci), natural penicillins generally are the drugs of choice for the treatment of infections caused by these organisms.
Because extended-spectrum penicillins are inactivated by staphylococcal penicillinases, the drugs are ineffective for the treatment of infections caused by penicillinase-producing S. aureus or S. epidermidis. Extended-spectrum penicillins have been used alone or in conjunction with an aminoglycoside for the treatment of genitourinary tract or intra-abdominal infections caused by susceptible strains of enterococci, including S. faecalis, but are not considered drugs of choice for these infections.
Gram-negative Aerobic Bacterial Infections
Infections Caused by Enterobacteriaceae
Extended-spectrum penicillins have been effective when used alone in the treatment of respiratory tract infections, urinary tract infections, intra-abdominal infections, skin and skin structure infections, bone and joint infections, and septicemia caused by susceptible Enterobacteriaceae. Ticarcillin may be effective in the treatment of infections caused by Proteus vulgaris, Providencia rettgeri (formerly Proteus rettgeri), Providencia stuartii, Morganella morganii (formerly Proteus morganii), P. mirabilis, Acinetobacter, Serratia, and some strains of Escherichia coli and Enterobacter. In the initial treatment of serious infections caused by Enterobacteriaceae, many clinicians suggest that an extended-spectrum penicillin or a third generation cephalosporin be used in conjunction with an aminoglycoside pending results of in vitro susceptibility tests.
Oral carbenicillin indanyl sodium has been used with some success for short-term therapy or long-term suppressive therapy in the treatment of acute or chronic infections of the upper and lower urinary tract or for asymptomatic bacteriuria caused by susceptible strains of Enterobacter, E. coli, M. morganii, P. mirabilis, P. vulgaris, and P. rettgeri or susceptible strains of Ps. aeruginosa and enterococci; however, the drug is not considered a drug of choice for the treatment of these infections. Oral carbenicillin indanyl sodium has been used with some success for the treatment of acute or chronic prostatitis caused by susceptible strains of Enterobacter, E. coli, P. mirabilis, or enterococci. Oral carbenicillin indanyl sodium also may be effective in the treatment of infections caused by Serratia.
Pseudomonal Infections
Ticarcillin has been effective when used alone or in conjunction with other anti-infectives for the treatment of infections caused by Ps. aeruginosa. Although there is some evidence that therapy with an extended-spectrum penicillin used alone may be as effective as combination therapy with an extended-spectrum penicillin and an aminoglycoside in the treatment of infections caused by susceptible Ps. aeruginosa, many clinicians state that concomitant therapy with an aminoglycoside should probably be used for the initial treatment of serious infections caused by or suspected of being caused by Ps. aeruginosa. Extended-spectrum penicillins are used alone or in conjunction with an aminoglycoside for the treatment of acute exacerbations of bronchopulmonary Ps. aeruginosa infections in children and adults with cystic fibrosis.
Ticarcillin also has been administered as an aerosol for long-term prophylaxis of acute exacerbations of these infections in patients with cystic fibrosis. (See Prophylaxis in Cystic Fibrosis Patients in Uses: Prophylaxis.) Although anti-infective therapy in patients with cystic fibrosis may result in clinical improvement and Ps. aeruginosa may be temporarily cleared from the sputum, a bacteriologic cure is rarely obtained and cannot be expected.
Extended-spectrum penicillins have been effective when used alone for the treatment of acute exacerbations of bronchopulmonary infections in cystic fibrosis patients, but emergence of resistant Ps. aeruginosa has been reported more frequently when the drugs were used alone than when the drugs were used in conjunction with an aminoglycoside. Because pharmacokinetic studies using ticarcillin indicate that patients with cystic fibrosis eliminate these drugs at a faster rate than do healthy individuals, some clinicians recommend that maximum dosages of extended-spectrum penicillins be used in cystic fibrosis patients. Ticarcillin has been administered by aerosol inhalation in conjunction with parenteral administration of the drug for the treatment of respiratory tract infections caused by Ps. aeruginosa. However, the value of aerosolized anti-infective therapy has not been established and there are no controlled studies to date that indicate whether concomitant aerosol inhalation and parenteral therapy is more effective for these infections than parenteral anti-infective therapy alone. Extended-spectrum penicillins have been effective when used in conjunction with gentamicin or in conjunction with co-trimoxazole and rifampin for the treatment of infections caused by Ps. maltophilia.
Anaerobic and Mixed Aerobic-Anaerobic Bacterial Infections
Ticarcillin has been effective when used alone in the treatment of anaerobic and mixed aerobic-anaerobic bacterial infections including intra-abdominal infections, pleuropulmonary infections, and gynecologic infections such as endometritis, salpingitis, pelvic cellulitis, and acute pelvic inflammatory disease (PID); however, the fixed-combination preparation containing ticarcillin disodium and clavulanate potassium or the fixed-combination preparation containing piperacillin sodium and tazobactam sodium may be preferred over the single-entity preparation for the treatment of these infections.
For initial treatment of life-threatening sepsis in adults, some clinicians recommend use of a third or fourth generation cephalosporin (cefotaxime, ceftriaxone, cefepime), ticarcillin disodium and clavulanate potassium, piperacillin sodium and tazobactam sodium, or imipenem (or meropenem) given in conjunction with an aminoglycoside. For intra-abdominal or pelvic infections likely to involve anaerobes, some clinicians recommend a regimen of ticarcillin disodium and clavulanate potassium, piperacillin sodium and tazobactam sodium, ampicillin sodium and sulbactam sodium, imipenem (or meropenem), cefoxitin, or cefotetan given with or without an aminoglycoside.
When the source of the bacteremia is suspected to be the biliary tract, some clinicians prefer piperacillin sodium and tazobactam sodium or ampicillin sodium and sulbactam sodium given with or without an aminoglycoside. Although clindamycin or metronidazole usually are considered the drugs of choice for the treatment of intra-abdominal or gynecologic infections caused by Bacteroides, ticarcillin disodium and clavulanate potassium or piperacillin sodium and tazobactam sodium are recommended as alternatives.
Meningitis and Other CNS Bacterial Infections
Ticarcillin has been effective when used in children or adults for the treatment of meningitis caused by susceptible H. influenzae, N. meningitidis, S. pneumoniae, Enterobacteriaceae, or Pseudomonas. However, penicillin G generally is considered the drug of choice for the treatment of meningitis caused by N. meningitidis and penicillin-susceptible S. pneumoniae, and ceftriaxone or cefotaxime generally are considered the drugs of choice for the treatment of meningitis caused by susceptible S. pneumoniae or H. influenzae. Extended-spectrum penicillins should not be used in the treatment of meningitis caused by ampicillin-resistant H. influenzae since these organisms usually are resistant to the drugs. In addition, when gram-negative bacillary meningitis is indicated by Gram stain or culture and in vitro susceptibility data are not yet available, many clinicians prefer to initiate therapy with a third generation cephalosporin (e.g., cefotaxime, ceftizoxime) in conjunction with IV and/or intrathecal aminoglycoside therapy. If the infection is found to be caused by Acinetobacter or Pseudomonas, some clinicians suggest that the treatment of choice is ceftazidime and an aminoglycoside.
Empiric Therapy in Febrile Neutropenic Patients
Extended-spectrum penicillins have been used for empiric anti-infective therapy in febrile neutropenic patients. Although extended-spectrum penicillins have been used alone for the treatment of infections in granulocytopenic patients, use of a single anti-infective agent in these patients has been associated with a low response rate and a high rate of emergence of resistant organisms.
Therefore, monotherapy with an extended-spectrum penicillin for empiric therapy in febrile neutropenic patients is not recommended, and these drugs usually are administered in conjunction with an aminoglycoside or another b-lactam antibiotic (e.g., a third generation cephalosporin). Results of controlled studies generally indicate that regimens that include an extended-spectrum penicillin and an aminoglycoside are as effective for empiric anti-infective therapy in granulocytopenic patients as regimens that include an extended-spectrum penicillin and a third generation cephalosporin or regimens that include an aminoglycoside and another b-lactam antibiotic (e.g., a third generation cephalosporin).
Results of several studies indicate that amikacin, gentamicin, netilmicin (no longer commercially available in the US), and tobramycin are equally effective when used in conjunction with an extended-spectrum penicillin in granulocytopenic patients and, if an extended-spectrum and aminoglycoside regimen is used, the specific aminoglycoside used should be based on the current pattern of resistance in each hospital.
Successful treatment of infections in granulocytopenic patients requires prompt initiation of empiric anti-infective therapy (even when fever is the only symptom or sign of infection) and appropriate modification of the initial regimen if the duration of fever and neutropenia is protracted, if a specific site of infection is identified, or if organisms resistant to the initial regimen are present.
The initial empiric regimen should be chosen based on the underlying disease and other host factors that may affect the degree of risk and on local epidemiologic data regarding usual pathogens in these patients and data regarding their in vitro susceptibility to available anti-infective agents. The fact that gram-positive bacteria have become a predominant pathogen in febrile neutropenic patients should be considered when selecting an empiric anti-infective regimen.
Regimens generally recommended for empiric therapy in febrile neutropenic patients with presumed bacterial infections include monotherapy with a third or fourth generation cephalosporin (e.g., ceftazidime, cefepime) or a carbapenem (e.g., imipenem and cilastatin sodium, meropenem); combination therapy consisting of a β-lactam antibiotic (e.g., ceftazidime, ceftriaxone), a carbapenem (e.g., imipenem, meropenem), an extended-spectrum penicillin (e.g., ticarcillin), or a fixed combination of an extended-spectrum penicillin and a b-lactamase inhibitor (e.g., piperacillin sodium and tazobactam sodium, ticarcillin disodium and clavulanate potassium) given in conjunction with an aminoglycoside (e.g., amikacin, gentamicin, netilmicin, tobramycin).
There are advantages and disadvantages to each of these strategies, and no empiric regimen has been identified that would be appropriate for all patients. Published protocols for the treatment of infections in febrile neutropenic patients should be consulted for specific recommendations regarding selection of the initial empiric regimen, when to change the initial regimen, and duration of therapy in these patients.
Prophylaxis
Perioperative Prophylaxis
Ticarcillin has been used perioperatively to reduce the incidence of infection in patients undergoing contaminated or potentially contaminated surgical procedures, including gynecologic and obstetric surgery (e.g., vaginal or abdominal hysterectomy, cesarean section), intra-abdominal or gastroduodenal surgery, or extensive surgery for cancer in the head and neck. Ticarcillin disodium and clavulanate potassium also has been used for perioperative prophylaxis in patients undergoing colorectal surgery.
Although extended-spectrum penicillins may be effective for prophylaxis in these patients, the drugs are not considered regimens of choice for such perioperative prophylaxis. In one controlled study, oral carbenicillin indanyl sodium administered perioperatively to patients undergoing transrectal biopsy of the prostate reduced the incidence of postoperative bacteriuria in these patients. Piperacillin sodium and tazobactam sodium also has been used for prophylaxis in patients undergoing urologic surgery. However, extended-spectrum penicillins are not considered drugs of choice for such prophylaxis.
Many clinicians do not recommend antimicrobial prophylaxis for patients with sterile urine undergoing most urologic procedures since the risk of serious infection is considered low; however, 331, 332 when preoperative urine cultures are positive or unavailable, anti-infective therapy should be administered to sterilize the urine prior to surgery or a single preoperative dose of an appropriate anti-infective agent should be used for perioperative prophylaxis.
Prophylaxis also is recommended before transrectal prostatic biopsies since urosepsis has occurred. If anti-infective prophylaxis is used in patients considered at high risk for postoperative bacteriuria (e.g., those with prolonged postoperative catheterization, positive urine cultures, or in hospitals with infection rates greater than 20%), some clinicians recommend use of co-trimoxazole, lomefloxacin, or cefazolin.
Other clinicians suggest preoperative use of ciprofloxacin in patients undergoing transrectal prostatic biopsy or those with a preoperative urinary catheter or urine cultures that are positive or unavailable.
Prophylaxis in Cystic Fibrosis Patients
Ticarcillin has been administered in conjunction with gentamicin or tobramycin as an aerosol for long-term prophylaxis of acute exacerbations of bronchopulmonary Ps. aeruginosa infections in patients with cystic fibrosis. Preliminary data indicate that oral inhalation of ticarcillin in conjunction with gentamicin or tobramycin twice daily may reduce the frequency of acute hospital admissions in these patients. However, further study is needed to evaluate efficacy and safety of prophylactic use of anti-infective aerosols in cystic fibrosis patients, and the possibility that long-term use of these aerosols may result in emergence of resistant strains of Ps. aeruginosa should be considered.
Dosage and Administration
Administration
Carbenicillin indanyl sodium is administered orally. Ticarcillin disodium is administered by slow IV injection or infusion or by deep IM injection. The fixed-combination preparation of ticarcillin disodium and clavulanate potassium and the fixed-combination preparation of piperacillin sodium and tazobactam sodium are administered by IV infusion.
Dosage in Renal Impairment
In patients with renal impairment, doses and/or frequency of administration of extended-spectrum penicillins must generally be modified in response to the degree of renal impairment.
Cautions
The most frequent adverse reactions to extended-spectrum penicillins include hypersensitivity reactions, GI effects, and local reactions. Other reported adverse effects of the drugs generally are mild and infrequent unless high dosages are used in patients with renal impairment.
Sensitivity Reactions
Hypersensitivity reactions reported with extended-spectrum penicillins are similar to those reported with other penicillins; however, severe hypersensitivity reactions have been reported less frequently with extended-spectrum penicillins than with natural penicillins.
Hypersensitivity reactions to extended-spectrum penicillins are manifested most frequently as rash, fever, and eosinophilia. Eosinophilia has been reported in patients receiving extended-spectrum penicillins. Morbilliform, maculopapular, or urticarial rash has been reported in 1-4% of patients receiving an extended-spectrum penicillin. Positive direct antiglobulin (Coombs’) test results have been reported rarely with carbenicillin and piperacillin.
Anaphylaxis has been reported rarely with carbenicillin, piperacillin, and ticarcillin. If a severe hypersensitivity reaction occurs during therapy with an extended-spectrum penicillin, the drug should be discontinued and the patient given appropriate treatment (e.g., epinephrine, corticosteroids, maintenance of an adequate airway, oxygen) as indicated. A higher incidence of hypersensitivity reactions (e.g., fever, rash, angioedema, anaphylaxis) reportedly occurs in patients with cystic fibrosis receiving extended-spectrum penicillins than in other patients receiving the drugs. It has been suggested that cystic fibrosis patients are at increased risk for hypersensitivity reactions to penicillins since they receive greater cumulative exposure to the drugs than other patients and have a high rate of generalized immune responsiveness and atopy.
For a more complete discussion on manifestations of penicillin hypersensitivity and information on the mechanisms of these reactions, the management of patients with hypersensitivity reactions, and how to identify patients at risk for hypersensitivity reactions to penicillins, see Cautions: Hypersensitivity Reactions, in the Natural Penicillins General Statement 8:12.16.04.
Hematologic Effects
In addition to eosinophilia and hemolytic anemia (see Cautions: Hypersensitivity Reactions), other adverse hematologic effects including transient neutropenia, leukopenia, granulocytopenia, anemia, and thrombocytopenia have been reported rarely with extended-spectrum penicillins. Leukopenia or neutropenia has been reported most frequently when high dosages of the drugs were administered for prolonged periods to patients with renal impairment.
These adverse hematologic effects generally are reversible following discontinuance of the drugs, but may recur with subsequent penicillin therapy. Although these adverse hematologic effects have been considered hypersensitivity reactions to penicillins, an immunologic mechanism has not been definitely established. Rarely, coagulation disorders manifested by abnormalities in coagulation tests, with or without clinical bleeding, have been reported with extended-spectrum penicillins.
Prolonged bleeding time, prolonged prothrombin time, abnormal platelet aggregation, purpura, and bleeding from the GI tract, mucous membranes, injection sites, or surgical wounds have been reported occasionally in patients receiving IV carbenicillin (no longer commercially available in the US) or IV ticarcillin. These adverse effects have been reported most frequently and were most severe when high dosages of the drugs were administered to patients with renal impairment; however, they have also been reported when usual dosages were used in patients with normal renal function.
Abnormal platelet aggregation, prolonged bleeding time, and bleeding also have been reported with usual dosages of piperacillin, but less frequently than with usual dosages of IV ticarcillin.Prolongation of bleeding time and abnormal platelet aggregation appear to be related to the dose and duration of therapy with the drugs. If prolongation of bleeding time occurs during therapy with an extended-spectrum penicillin, it is usually evident 3-12 days after initiation of therapy and returns to pretreatment levels 2-7 days after discontinuance of the drug.
Patients with preexisting thrombocytopenia (e.g., induced by antineoplastic chemotherapy), prolonged prothrombin time, platelet dysfunction, and/or azotemia appear to be at increased risk of penicillin-induced coagulation disorders. In vitro studies using IV carbenicillin (no longer commercially available in the US), piperacillin, and ticarcillin indicate that the drugs interfere with adenosine diphosphate-induced, collagen-induced, and epinephrine-induced platelet aggregation. There is some evidence that carbenicillin may also interfere with the conversion of fibrinogen to fibrin.
GI Effects
Oral carbenicillin indanyl sodium occasionally causes dose-related nausea, vomiting, diarrhea, abdominal cramps, and flatulence. Dry mouth, bad taste, glossitis, furry tongue, anorexia, rectal bleeding, and vaginitis have also been reported rarely with the drug. Carbenicillin indanyl sodium has a bitter taste and, although commercially available tablets of the drug are film-coated, patients receiving the drug generally complain of an unpleasant aftertaste and smell. Parenteral administration of piperacillin or ticarcillin occasionally results in adverse GI effects including nausea, loose stools, and diarrhea. Loose stools or diarrhea has been reported in up to 3% of patients receiving piperacillin. Clostridium difficile-associated diarrhea and colitis (also known as antibiotic-associated pseudomembranous colitis), caused by toxin-producing clostridia, has been reported with the use of anti-infective agents including carbenicillin indanyl sodium, ticarcillin and clavulanate potassium, and ticarcillin disodium.
Colitis may occur during or following discontinuance of anti-infective therapy and ranges in severity from mild to life-threatening. Mild cases of colitis may respond to discontinuance of the drug alone, but diagnosis and management of moderate to severe cases should include appropriate bacteriologic studies and treatment with fluid, electrolyte, and protein supplementation as indicated; rarely, cautious use of sigmoidoscopy (or other appropriate endoscopic examination) may be considered necessary. If colitis is moderate to severe and is not relieved by discontinuance of the drug, appropriate anti-infective therapy (e.g., oral metronidazole or vancomycin) should be administered.
Renal, Electrolyte, and Genitourinary Effects
Acute interstitial nephritis, manifested as rash, hematuria, cylindruria, eosinophilia, and renal failure, has been reported rarely with carbenicillin and piperacillin. The nephritis appears to be a hypersensitivity reaction to the drug.
For more information on penicillin-induced acute interstitial nephritis, seeCautions: Renal Effects, in the Penicillinase-Resistant Penicillins General Statement 8:12.16.12. Hypokalemia, sometimes associated with metabolic alkalosis, has been reported rarely with carbenicillin, piperacillin, and ticarcillin. In most reported cases, hypokalemia responded to oral or IV potassium supplements given during or after completion of penicillin therapy; only rarely was hypokalemia severe enough to require discontinuance of the drugs. Although it has been suggested that hypokalemia during penicillin therapy may be the result of redistribution of potassium within the body, hypokalemia appears to be related to the fact that penicillins act as nonabsorbable anions in the distal renal tubules and therefore promote urinary loss of potassium.
Because acylaminopenicillins are commercially available as monosodium salts, they contain less than half the sodium content of a-carboxypenicillins which are commercially available as disodium salts. Although there are no controlled comparative studies to date, theoretically, the risk of hypokalemia or fluid overload should be less with piperacillin than with ticarcillin. Hemorrhagic cystitis, manifested as erythrocyturia with frequent and painful voiding, has been reported in several children receiving IV carbenicillin (no longer commercially available in the US).
This adverse genitourinary effect may be caused by direct irritation by the drugs on the bladder mucosa rather than a hypersensitivity reaction since it was not associated with eosinophilia or fever. Transient microscopic hematuria has also been reported in at least one child receiving IV ticarcillin. Although the clinical importance is unclear, transient increases in serum concentrations of creatinine and BUN have been reported with piperacillin.
Hepatic Effects
Transient increases in serum concentrations of AST (SGOT), ALT (SGPT),LDH, alkaline phosphatase, and bilirubin have been reported with oral carbenicillin indanyl sodium and parenteral piperacillin and ticarcillin. In most reported cases, increased serum concentrations of liver enzymes were not associated with hepatotoxicity and returned to pretreatment concentrations when the drugs were discontinued. Reversible hepatitis characterized by nausea, vomiting, and a tender, slightly enlarged liver with spotty liver cell necrosis but no cholestasis has been reported rarely with IV carbenicillin. Transient hepatitis and cholestatic jaundice have occurred rarely during IV ticarcillin disodium and clavulanate potassium therapy. Although a causal relationship has not been definitely established, cholestatic hepatitis has been reported in at least one patient who received IV piperacillin.
Nervous System Effects
Adverse nervous system effects including lethargy, myoclonic and other seizures, hyperreflexia, asterixis, and stupor have occurred following parenteral administration of ticarcillin especially when large IV dosages of the drug were administered to patients with impaired renal function. Headache, dizziness, fatigue, and seizures also have been reported rarely with piperacillin. These neurotoxic reactions are similar to those reported with large IV dosages of IV penicillin G3, 46, 179 and appear to be associated with high CNS concentrations of the drugs. For further information on adverse nervous system effects associated with penicillins, see Cautions: Nervous System and Neurovascular Effects, in the Natural Penicillins General Statement 8:12.16.04.
Local Effects
Local reactions, which may occasionally be severe enough to require discontinuance of the drug, are among the most frequent adverse effects of parenterally administered extended-spectrum penicillins. IV administration of piperacillin and ticarcillin has resulted in vein irritation, pain, erythema, phlebitis, and thrombophlebitis. Ecchymosis, deep-vein thrombosis, and hematoma have also occurred rarely with IV piperacillin. Adverse local effects occur most frequently when IV therapy is prolonged, when IV sites are not changed regularly, and when high concentrations of the drugs are used. These effects are reported in 3-5% of patients receiving IV piperacillin and 2-9% of patients receiving IV ticarcillin. IM administration of ticarcillin may cause pain, induration, or erythema at the site of injection. Administering the drugs slowly (over 12-15 seconds) may minimize pain associated with IM administration. IM administration of the drugs is also less painful if they are reconstituted with lidocaine hydrochloride (without epinephrine) or bacteriostatic water containing benzyl alcohol; however, bacteriostatic water containing benzyl alcohol should not be used to reconstitute IM injections for use in neonates. (See Cautions: Pediatric Precautions.)
Precautions and Contraindications
Carbenicillin, piperacillin, and ticarcillin are contraindicated in patients who are hypersensitive to any penicillin. Prior to initiation of therapy with an extended-spectrum penicillin, careful inquiry should be made concerning previous hypersensitivity reactions to penicillins, cephalosporins, or other drugs. There is clinical and laboratory evidence of partial cross-allergenicity among penicillins and other b-lactam antibiotics including cephalosporins and cephamycins.
Although it has not been proven that allergic reactions to antibiotics are more frequent in atopic individuals, the manufacturers state that extended-spectrum penicillins should be used with caution in patients with a history of allergy, particularly to drugs. For more information on hypersensitivity reactions to penicillins and precautions associated with these reactions, see Cautions: Hypersensitivity Reactions in the Natural Penicillins General Statement 8:12.16.04. Renal, hepatic, and hematologic systems should be evaluated periodically during prolonged therapy with extended-spectrum penicillins.
Although hypokalemia has only been reported rarely with extended-spectrum penicillins, serum electrolytes should be monitored and the possibility of hypokalemia should be considered during prolonged therapy with the drugs, especially in patients with fluid and electrolyte imbalance or low potassium reserves and in patients who are receiving cytotoxic therapy or diuretics.
The possibility of sodium overload should also be considered when the drugs are administered to patients whose sodium intake is restricted, and cardiac status and serum electrolytes should be monitored during therapy in these patients. Because C. difficile-associated diarrhea and colitis has been reported with the use of anti-infective agents including carbenicillin indanyl sodium, piperacillin sodium and tazobactam sodium, ticarcillin and clavulanate potassium, and ticarcillin disodium, it should be considered in the differential diagnosis of patients who develop diarrhea during therapy with these anti-infectives.
Because bleeding complications have been reported rarely during therapy with some extended-spectrum penicillins (see Cautions: Hematologic Effects), the possibility that these reactions could occur should be considered during therapy with the drugs, especially when high dosages are used in patients with renal impairment.
If bleeding manifestations occur, the drugs should be discontinued and appropriate therapy instituted. Use of extended-spectrum penicillins may result in overgrowth of nonsusceptible organisms including fungi. Superinfection has been reported in up to 6-8% of patients receiving an extended-spectrum penicillin; the majority of superinfections are caused by Pseudomonas, Serratia, Klebsiella, or Candida.
Resistant strains of some organisms, especially Ps. aeruginosa, have developed during therapy with extended-spectrum penicillins. The use of indwelling catheters contributes to the occurrence of superinfections during therapy with the drugs and should be avoided if possible. Careful observation of the patient during therapy with an extended-spectrum penicillin is essential. If suprainfection or superinfection occurs, the drug should be discontinued and appropriate therapy instituted. Because serum concentrations of extended-spectrum penicillins are higher and more prolonged in patients with renal impairment than in patients with normal renal function, dose and/or frequency of administration of the drugs should be decreased in patients with impaired renal function.
Pediatric Precautions
Safe use of carbenicillin indanyl sodium in children has not been definitely established. Ticarcillin disodium has been used safely and effectively in neonates and children. The manufacturer of piperacillin sodium and tazobactam sodium states that safety and efficacy of the drug in children younger than 12 years of age have not been established. Safety and efficacy of ticarcillin disodium and clavulanate potassium in children younger than 3 months of age have not been established. Extended-spectrum penicillins that have been reconstituted for IM use with bacteriostatic water for injection containing benzyl alcohol should not be used in neonates. Although a causal relationship has not been established, administration of injections preserved with benzyl alcohol has been associated with toxicity in neonates. Toxicity appears to have resulted from administration of large amounts (i.e., about 100-400 mg/kg daily) of benzyl alcohol in these neonates.
Mutagenicity and Carcinogenicity
The mutagenic and carcinogenic potentials of extended-spectrum penicillins have not been fully determined to date.
Pregnancy, Fertitlity and Lactation
Safe use of carbenicillin, ticarcillin, piperacillin sodium and tazobactam sodium, or ticarcillin disodium and clavulanate potassium during pregnancy has not been definitely established. Reproduction studies in mice and rats using piperacillin doses up to 4 times the usual human dose have not revealed evidence of impaired fertility or harm to the fetus. However, ticarcillin has been shown to be teratogenic in mice when given in doses equivalent to the usual human dose. There are no adequate or controlled studies to date using extended-spectrum penicillins in pregnant women, and the drugs should be used during pregnancy only when clearly needed. Because carbenicillin, piperacillin and ticarcillin are distributed into milk, the drugs should be used with caution in nursing women.
Drug Interactions
For further information on these and other drug interactions reported with penicillins, see Drug Interactions in the Natural Penicillins General Statement 8:12.16.04. Although not all drug interactions reported with other penicillins have been reported with extended-spectrum penicillins, the fact that some of these interactions could occur with these drugs should be considered.
Aminoglycosides
Synergism with Aminoglycosides
The antibacterial activity of extended-spectrum penicillins and aminoglycosides is additive or synergistic in vitro against some strains of Pseudomonas aeruginosa. The synergistic effect of extended-spectrum penicillins and aminoglycosides is used to therapeutic advantage in the treatment of infections caused by Ps. aeruginosa, especially in febrile granulocytopenic patients or patients with cystic fibrosis, and may be associated with a higher response rate and a lower rate of emergence of resistant organisms compared with therapy with an extended-spectrum penicillin alone. However, synergism between extended-spectrum penicillins and aminoglycosides generally is unpredictable and antagonism has been reported rarely in vitro when extended-spectrum penicillins were used in conjunction with amikacin, gentamicin, or tobramycin.
Therefore, some clinicians suggest that when concomitant therapy is indicated it may be advisable to use appropriate in vitro studies to demonstrate synergism against the isolated organism. In vitro studies indicate that extended-spectrum penicillins and aminoglycosides also exert a synergistic bactericidal effect against some Enterobacteriaceae (e.g., Escherichia coli, Klebsiella, Citrobacter, Enterobacter, Serratia, Proteus mirabilis).
Although the clinical importance has not been determined, partial synergism has also been reported in vitro against Acinetobacter calcoaceticus when carbenicillin, or piperacillin was used in conjunction with an aminoglycoside. Although the effect is probably not clinically important, a synergistic bactericidal effect has been reported in vitro against some strains of enterococci when carbenicillin or ticarcillin was used in conjunction with an aminoglycoside. In one in vitro study, piperacillin used in conjunction with gentamicin exerted a synergistic effect against some strains of S. aureus and an indifferent or additive effect against enterococci.
Incompatibility with Aminoglycosides
Extended-spectrum penicillins are physically and/or chemically incompatible with aminoglycosides and can inactivate the drugs in vitro. The extent of in vitro inactivation of aminoglycosides by penicillins depends on the specific drugs involved and appears to be directly proportional to the penicillin concentration, length of exposure, and temperature. Of the currently available aminoglycosides, amikacin generally is the least susceptible and tobramycin is the most susceptible to inactivation by penicillins.
Most in vitro studies indicate that carbenicillin (parenteral formulation no longer commercially available in the US) inactivates aminoglycosides at a faster rate than piperacillin or ticarcillin. In vitro inactivation of aminoglycosides by extended-spectrum penicillins can occur if the drugs are administered in the same syringe or IV infusion container; therefore, when concomitant therapy is indicated, in vitro mixing of extended-spectrum penicillins and aminoglycosides should be avoided. In vitro inactivation of aminoglycosides by extended-spectrum penicillins also occurs in serum samples obtained from patients receiving concomitant therapy with the drugs.
This could adversely affect results of serum aminoglycoside assays performed on the serum samples. (See Laboratory Test Interferences: Serum Aminoglycoside Assays.) Extended-spectrum penicillins also can inactivate aminoglycosides in vivo.
In patients with impaired renal function, concomitant administration of carbenicillin, ticarcillin, or piperacillin and gentamicin has resulted in decreased serum aminoglycoside concentrations and serum half-lives compared with administration of the aminoglycoside alone. Although this effect has been reported principally in patients with renal impairment when elimination of the drugs is delayed and high concentrations may accumulate, in vivo inactivation of aminoglycosides has been reported in a few patients with normal renal function receiving concomitant therapy with carbenicillin or ticarcillin and gentamicin or tobramycin.
Some clinicians recommend that serum aminoglycoside concentrations be monitored more closely than usual in patients receiving concomitant penicillin therapy, especially when high dosages of the penicillin are administered or when the patient has impaired renal function. Because amikacin appears to be more resistant than other currently available aminoglycosides to in vitro inactivation by penicillins, some clinicians recommend that this aminoglycoside be used when concomitant penicillin and aminoglycoside therapy is indicated, especially in patients with impaired renal function.
β-Lactam Antibiotics
Some in vitro studies indicate that the antibacterial activity of extended-spectrum penicillins may be additive or partially synergistic with other b-lactam antibiotics (e.g., cephalosporins, cephamycins). However, synergism between b-lactam antibiotics is generally unpredictable and indifference or antagonism has been reported more frequently than synergism with these combinations. Extended-spectrum penicillins have been used concomitantly with cephalosporins with no apparent decrease in activity. The mechanism of synergism between b-lactam antibiotics has not been fully determined, but synergism may occur because the drugs bind to different penicillin-binding proteins (PBPs) or because one b-lactam antibiotic inhibits b-lactamases that could hydrolyze the other b-lactam antibiotic.
Antagonism between b-lactam antibiotics may occur if one of the drugs induces b-lactamase production in the bacteria or if competition for or alteration of the PBPs occurs. In vitro, combinations of piperacillin with cefazolin, cefotaxime, or ceftizoxime have been additive or synergistic against some strains of Ps. aeruginosa and Enterobacteriaceae; however, in vitro antagonism has also been reported with these combinations. In one study which used carbenicillin or piperacillin in conjunction with cefoxitin, synergism occurred with these drugs against B. fragilis, but antagonism occurred against Enterobacteriaceae.
Clavulanic Acid
In vitro studies indicate that the combination of carbenicillin, ticarcillin, or piperacillin with clavulanic acid, a b-lactamase inhibitor, results in a synergistic bactericidal effect against many strains of b-lactamase-producing bacteria. This synergism occurs because clavulanic acid has a high affinity for and irreversibly binds to certain b-lactamases that can inactivate extended-spectrum penicillins. Concomitant clavulanic acid does not result in a synergistic effect with extended-spectrum penicillins against resistant organisms if intrinsic resistance rather than b-lactamase production is involved.
The fact that concomitant use of clavulanic acid broadens the spectrum of activity of extended-spectrum penicillins is used to therapeutic advantage in the treatment of infections that may be caused by b-lactamase-producing organisms which are resistant to extended-spectrum penicillins. Ticarcillin is commercially available in a fixed-ratio combination with clavulanate potassium for parenteral use. For a complete discussion of this fixed-combination preparation, see Ticarcillin Disodium and Clavulanate Potassium 8:12.16.16.
Tazobactam Sodium
In vitro studies indicate that the combination of carbenicillin, ticarcillin, or piperacillin with tazobactam, a b-lactamase inhibitor, results in synergistic bactericidal activity against many strains of b-lactamase producing bacteria.
This synergism occurs because tazobactam has a high affinity for and irreversibly binds to certain b-lactamases that can inactivate extended-spectrum penicillins. Concomitant use of tazobactam sodium does not result in a synergistic effect with extended-spectrum penicillins against resistant organisms if intrinsic resistance rather than b-lactamase production is involved. The fact that concomitant use of tazobactam broadens the spectrum of activity of extended-spectrum penicillins is used to therapeutic advantage in the treatment of infections that may be caused by b-lactamase-producing organisms that are resistant to extended-spectrum penicillins. Piperacillin is commercially available in a fixed-ratio combination with tazobactam sodium for parenteral use. For further discussion of this fixed-combination preparation, see Piperacillin Sodium and Tazobactam Sodium 8:12.16.16.
Probenecid
Oral probenecid administered shortly before or simultaneously with extended-spectrum penicillins slows the rate of renal tubular secretion of the penicillins and produces higher and prolonged serum concentrations of the drugs. Studies using carbenicillin, piperacillin, and ticarcillin indicate that peak serum concentrations and serum half-lives of these drugs generally are increased by 24-75% and areas under the serum concentration-time curves (AUCs) may be increased by 60-124% when oral probenecid is administered concomitantly. Studies using piperacillin indicate that probenecid also decreases the volumes of distribution of this penicillin by 20-35% which may contribute to higher serum concentrations of the drugs. However, concomitant oral probenecid reportedly increased the volumes of distribution of carbenicillin and ticarcillin in one study. Concomitant administration of probenecid also reportedly increases CSF concentrations of extended-spectrum penicillins.
Lithium
Because changes in sodium intake may alter renal elimination of lithium and affect the therapeutic response to lithium and because of the relatively high sodium content of commercially available ticarcillin disodium, serum lithium concentrations probably should be monitored more frequently than usual if this extended-spectrum penicillin is administered to a patient receiving lithium.
Methotrexate
Concomitant use of penicillins (e.g., amoxicillin, carbenicillin) may decrease renal clearance of methotrexate, presumably by inhibiting renal tubular secretion of the drug. Increased serum concentrations of methotrexate, resulting in GI or hematologic toxicity, have been reported in patients receiving concomitant administration of high- or low-dose methotrexate therapy with penicillins. Patients receiving penicillins and methotrexate concomitantly should be monitored carefully.
Vecuronium Bromide
Intraoperative administration of acylaminopenicillins, including piperacillin, reportedly prolongs vecuronium bromide-induced neuromuscular blockade, increasing the duration of skeletal muscle relaxation by an average of 40-55%. Acylaminopenicillins should be used perioperatively with caution in patients receiving vecuronium bromide, and the possibility of prolonged neuromuscular blockade should be considered.
Laboratory Test Interferences
For more complete information on these and other laboratory test interferences reported with penicillins, see Laboratory Test Interferences in the Natural Penicillins General Statement 8:12.16.04. Although not all laboratory test interferences reported with other penicillins have been reported with extended-spectrum penicillins, the possibility that these interferences could occur with these drugs should be considered.
Tests for Urinary and Serum Proteins
Like other penicillins, extended-spectrum penicillins interfere with or cause false-positive results in a variety of test methods used to determine urinary or serum proteins.
Tests for Urinary Glucose
Although studies using other extended-spectrum penicillins have not been reported to date, carbenicillin interferes with urinary glucose determinations using cupric sulfate (e.g., Benedict’s solution, Clinitest®). Glucose oxidase tests for urinary glucose (Clinistix®, Tes-Tape®) are reportedly unaffected by carbenicillin.
Tests for Uric Acid
Carbenicillin can cause falsely increased serum uric acid concentrations when the copper-chelate method is used; however, phosphotungstate and uricase methods for serum uric acid appear to be unaffected by the drug.
Immunohematology Tests
Positive direct antiglobulin (Coombs’) test results have been reported in patients receiving carbenicillin or piperacillin. This reaction may interfere with hematologic studies or transfusion cross-matching procedures and should be considered in patients receiving the drugs.
Serum Aminoglycoside Assays
Because extended-spectrum penicillins inactivate aminoglycosides in vitro (see Drug Interactions: Aminoglycosides), presence of the drugs in serum samples to be assayed for aminoglycoside concentrations may result in falsely decreased results.
The extent of in vitro inactivation of aminoglycosides by penicillins depends on the penicillin concentration, length of storage, and temperature, but a greater than 10% loss of aminoglycoside activity has been reported in serum samples stored for 8 hours or more at room temperature or 2-8°C. To ensure accurate serum aminoglycoside assays in patients receiving an extended-spectrum penicillin concomitantly with an aminoglycoside, penicillinase should be added to blood collection tubes whenever samples cannot be assayed immediately for aminoglycoside concentrations.
Some clinicians suggest that serum specimens from patients receiving concomitant penicillin and aminoglycoside therapy can be frozen at -20°C to avoid in vitro inactivation of the aminoglycoside if the sample cannot be assayed within a few hours; however, although freezing will minimize aminoglycoside inactivation by penicillins and may be sufficient for short-term storage of the samples, it does not totally prevent the interaction.
Other Laboratory Tests
Carbenicillin reportedly reacts with some, but not all, HLA antigens on cell membranes. If the drug is present in tissue specimens, it could interfere with HLA typing of the tissue by competing with HLA alloantiserum for binding sites. In one study, this effect also occurred with penicillin G, but not with ticarcillin. Mechanism of Action Extended-spectrum penicillins have a mechanism of action similar to that of other penicillins.
For information on the mechanism of action of penicillins, see Mechanism of Action in the Natural Penicillins General Statement 8:12.16.04.
Extended-spectrum penicillins are more active than natural penicillins, penicillinase-resistant penicillins, and aminopenicillins against gram-negative bacilli because extended-spectrum penicillins are more resistant to inactivation by b-lactamases produced by gram-negative bacteria and/or because they more readily penetrate the outer membranes of these organisms.
The greater ability of extended-spectrum penicillins to gain access to the target enzymes (penicillin-binding proteins) may be partly related to the presence of polar groups on the side chain at R on the penicillin nucleus.
Extended-spectrum penicillins reportedly vary in their rate of bactericidal action and in the completeness of this effect. This appears to result partly from differences in drug-induced morphologic effects on susceptible bacteria and subsequent formation of bacterial variants with varying degrees of osmotic stability. In vitro studies using susceptible strains of Pseudomonas aeruginosa indicate that ticarcillin causes rapid formation of spheroplasts which are unstable and lyse rapidly whereas acylureidopenicillins cause the formation of elongated or filamentous forms of the organism which are more stable and lyse at a slower rate.
Preliminary data indicate that acylureidopenicillins usually cause the formation of filamentous forms in susceptible gram-negative bacteria because these derivatives have a high affinity for penicillin-binding protein (PBP) 3 which appears to be responsible for septum formation in these organisms. Although the clinical importance of these differences in morphologic effects is unclear, results of in vitro studies with some bacteria (e.g., Escherichia coli) indicate that filamentous forms are capable of rapidly resuming growth if the penicillin is removed before the cells lyse. It has been suggested that the observation that acylaminopenicillins may not be as rapidly bactericidal as some other anti-infectives may have negative clinical implications in the use of the drugs in febrile granulocytopenic patients.
Spectrum Extended-spectrum penicillins are active in vitro against most gram-positive and gram-negative aerobic cocci (except penicillinase-producing strains), some gram-positive aerobic and anaerobic bacilli, and many gram-negative anaerobic bacilli. The drugs are also active against many gram-negative aerobic bacilli, including some Enterobacteriaceae and Pseudomonas that are resistant to other commercially available penicillins
. Extended-spectrum penicillins are inactive against mycobacteria, Mycoplasma, Rickettsia, fungi, and viruses. a-Carboxypenicillins (carbenicillin, ticarcillin) generally have the same spectra of activity and the same level of activity against susceptible organisms except that ticarcillin is more active in vitro on a weight basis than carbenicillin against susceptible Pseudomonas. Acylaminopenicillins (piperacillin) have a broader spectrum of activity than a-carboxypenicillins and are active against some gram-negative bacilli that are resistant to carbenicillin and ticarcillin. However, there are differences among the acylaminopenicillins in spectra of activity and levels of activity against susceptible organisms. Piperacillin generally is more active in vitro on a weight basis than a-carboxypenicillins against Enterobacteriaceae, but piperacillin generally is more active in vitro on a weight basis than other currently available extended-spectrum penicillins against Pseudomonas aeruginosa.
Fixed-ratio combinations of ticarcillin disodium and clavulanate potassium or piperacillin sodium and tazobactam sodium are active in vitro against organisms susceptible to ticarcillin or piperacillin alone, respectively. In addition, because clavulanic acid or tazobactam can inhibit certain b-lactamases that generally inactivate ticarcillin or piperacillin, combinations of ticarcillin disodium and clavulanate potassium or of piperacillin sodium and tazobactam sodium are active in vitro against many b-lactamase-producing organisms that are resistant to ticarcillin or piperacillin alone. For further discussion of spectrum of activity of the fixed-combination preparation of ticarcillin disodium and clavulanate potassium, see Spectrum in Ticarcillin Disodium and Clavulanate Potassium in 8:12.16.04.
In Vitro Susceptibility Testing
Results of in vitro susceptibility tests with extended-spectrum penicillins may be affected by test media, period of incubation, inoculum size, and pH. Susceptibility testing for Ps. aeruginosa is particularly affected by inoculum size which may indicate that the isolates contain a mixture of susceptible and resistant strains.
Because there are differences between the spectra of activity of a-carboxypenicillins and acylaminopenicillins and because of differences in the degree of activity of the various drugs against susceptible bacteria, extended-spectrum penicillins should be tested individually to determine in vitro susceptibility regardless of whether the disk-diffusion procedure or other susceptibility testing procedures are used.
The National Committee for Clinical Laboratory Standards (NCCLS) states that if results of in vitro susceptibility testing indicate that a clinical isolate is susceptible to a particular extended-spectrum penicillin, then an infection caused by this strain may be appropriately treated with the dosage of the drug recommended for that type of infection and infecting species, unless otherwise contraindicated.
If results indicate that a clinical isolate has intermediate susceptibility to a particular extended-spectrum penicillin, then the strain has a minimum inhibitory concentration (MIC) that approaches usually attainable blood and tissue concentrations and response rates may be lower than for strains identified as susceptible. Therefore, the intermediate category implies clinical applicability in body sites where the drug is physiologically concentrated or when a high dosage of the drug is used. This intermediate category also includes a buffer zone which should prevent small, uncontrolled, technical factors from causing major discrepancies in interpretations, especially for drugs with narrow pharmacotoxicity margins. If results of in vitro susceptibility testing indicate that a clinical isolate is resistant to a particular extended-spectrum penicillin, the strain is not inhibited by systemic concentrations of the drug achievable with usual dosage schedules and/or MICs fall in the range where specific microbial resistance mechanisms are likely and efficacy has not been reliably demonstrated in clinical studies.
Disk Susceptibility Tests
There is no class disk that can be used in the disk-diffusion procedure to test susceptibility to all currently available extended-spectrum penicillins. Therefore, when this procedure is used to test susceptibility to extended-spectrum penicillins, individual disks must be used for the drugs. For information on use of the disk-diffusion procedure to test susceptibility to extended-spectrum penicillins and interpretation of test results, see Spectrum: In Vitro Susceptibility Testing, in the individual monographs in 8:12…
Dilution Susceptibility Tests
When dilution susceptibility testing (agar or broth dilution) is performed according to NCCLS standardized procedures using the individual extended-spectrum penicillins, Pseudomonas with MICs of 64 mcg/mL or less are susceptible to ticarcillin and those with MICs of 128 mcg/mL or greater are resistant to the drug. Urinary tract isolates of Ps. aeruginosa with MICs of 128 mcg/mL or less are considered susceptible to carbenicillin and those with MICs of 512 mcg/mL or greater are resistant to the drug. When testing susceptibility of Enterobacteriaceae according to NCCLS standardized procedures using the individual extended-spectrum penicillins, those with MICs of 16 mcg/mL or less are susceptible to carbenicillin (urinary tract isolates only) or ticarcillin. For further information on dilution susceptibility testing of extended-spectrum penicillins and interpretation of test results, see Spectrum: In Vitro Susceptibility Testing, in the individual monographs in 8:12.16.04.
Gram-positive Aerobic Bacteria
Extended-spectrum penicillins are active in vitro against many gram-positive aerobic cocci including nonpenicillinase-producing strains of Staphylococcus aureus and S. epidermidis; groups A, B, C, and G5, 49 streptococci; Streptococcus pneumoniae; viridans streptococci; and some strains of enterococci. In vitro, extended-spectrum penicillins reportedly are slightly more resistant than natural penicillins or aminopenicillins to inactivation by staphylococcal penicillinases; however, this is not clinically important and penicillinase-producing strains of S. aureus and S. epidermidis generally are resistant to the drugs.
Although extended-spectrum penicillins generally are more active in vitro than natural penicillins against enterococci, the drugs are less active than natural penicillins or aminopenicillins against most other susceptible gram-positive cocci. The MIC90 (minimum inhibitory concentration of the drug at which 90% of strains tested are inhibited) of carbenicillin, piperacillin, or ticarcillin reported for most nonpenicillinase-producing strains of S. aureus and S. epidermidis is 1-2 mcg/mL. In vitro, acylaminopenicillins generally are more active on a weight basis than a-carboxypenicillins against streptococci. The MIC90 of carbenicillin or ticarcillin reported for groups A, B, C, and G49 streptococci, S. pneumoniae, and viridans streptococci is 0.4-4 mcg/mL; the MIC90 of piperacillin reported for these organisms is 0.02-1 mcg/mL.
Susceptible strains of enterococci, including E. faecalis (formerly S. faecalis), generally are inhibited in vitro by piperacillin concentrations of 1.5-8 mcg/mL. Carbenicillin or ticarcillin concentrations of 2-50 mcg/mL generally are required for in vitro inhibition of E. faecalis. There is little published information on the activity of extended-spectrum penicillins against gram-positive aerobic bacilli. Carbenicillin concentrations of 0.25 mcg/mL reportedly inhibit some strains of Bacillus anthracis.
Carbenicillin, piperacillin, and ticarcillin reportedly have some in vitro activity against Listeria monocytogenes, although the drugs are less active against this organism than natural penicillins or aminopenicillins. A few strains of Nocardia are reportedly inhibited in vitro by ticarcillin concentrations of 25 mcg/mL; however, most strains of this organism are resistant to extended-spectrum penicillins.
Gram-negative Aerobic Bacteria
Neisseria Extended-spectrum penicillins generally are active in vitro against gram-negative aerobic cocci including many strains of Neisseria meningitidis and N. gonorrhoeae. N. meningitidis is generally inhibited in vitro by carbenicillin, piperacillin, or ticarcillin concentrations of 0.01-0.2 mcg/mL. Nonpenicillinase-producing strains of N. gonorrhoeae generally are inhibited by concentrations of extended-spectrum penicillins of 0.01-0.5 mcg/mL. Some strains of N. gonorrhoeae that are resistant to natural penicillins (including some penicillinase-producing strains) are inhibited in vitro by carbenicillin or ticarcillin concentrations of 0.5-16 mcg/mL or piperacillin concentrations of 0.25-2 mcg/mL.
Haemophilus
Extended-spectrum penicillins are active in vitro against some strains of Haemophilus influenzae. Susceptible strains of H. influenzae generally are inhibited in vitro by carbenicillin, piperacillin, or ticarcillin concentrations of 0.1-0.8 mcg/mL. Although a few b-lactamase-producing strains of H. influenzae are inhibited in vitro by carbenicillin, piperacillin, or ticarcillin concentrations of 4-32 mcg/mL, most b-lactamase-producing strains of H. influenzae and H. parainfluenzae are resistant to the drugs.
Enterobacteriaceae
Extended-spectrum penicillins are more active than other currently available penicillins against Enterobacteriaceae. a-Carboxypenicillins are active in vitro against some strains of Escherichia coli, Morganella morganii (formerly Proteus morganii), Proteus mirabilis, P. vulgaris, Providencia rettgeri (formerly Proteus rettgeri), Salmonella, and Shigella. Acylaminopenicillins generally are active against Enterobacteriaceae that are susceptible to a-carboxypenicillins and, in addition, are active in vitro against some strains of Citrobacter, Enterobacter,Klebsiella, and Serratia. In vitro, carbenicillin or ticarcillin concentrations of 12.-64 mcg/mL inhibit 43-80% of strains of E. coli tested; however, the MIC90 of the drugs reported for this organism is usually greater than 128 mcg/mL. The MIC90 of carbenicillin or ticarcillin reported for M. morganii, P. vulgaris, P. rettgeri, and P. stuartii is usually 1-32 mcg/mL and the MIC90 of the drugs reported for Proteus mirabilis is usually 0.8-4 mcg/mL.
Some strains of Citrobacter, Enterobacter, and Serratia are inhibited in vitro by carbenicillin or ticarcillin concentrations of 16-64 mcg/mL; however, the MIC90 of the drugs reported for these organisms is usually greater than 128 mcg/mL and many strains of these Enterobacteriaceae as well as most strains ofKlebsiella generally are considered resistant to a-carboxypenicillins. In vitro, piperacillin concentrations of 32-100 mcg/mL reportedly inhibit 50-75% of strains of E. coli tested. The MIC90 of piperacillin reported for Citrobacter is generally 6.3-50 mcg/mL and the MIC90 of the drugs reported for Enterobacter is generally 16-64 mcg/mL. Piperacillin concentrations of 16-64 mcg/mL generally inhibit 50-90% of strains of Klebsiella tested.
Piperacillin concentrations of 16-100 mcg/mL reportedly inhibit 50-90% of Serratia tested in vitro. Piperacillin concentrations of 1-16 mcg/mL generally inhibit 75-90% of M. morganii, P. vulgaris, and Providencia tested. In vitro, susceptible strains of Salmonella generally are inhibited by carbenicillin, piperacillin, or ticarcillin concentrations of 4-16 mcg/mL. The MIC90 of ticarcillin reported for Shigella is 2-4 mcg/mL and the MIC90 of carbenicillin or piperacillin reported for this organism is 32 mcg/mL.
Pseudomonas
Unlike natural penicillins, penicillinase-resistant penicillins, and aminopenicillins, extended-spectrum penicillins have some activity against Pseudomonas, but the in vitro activity of extended-spectrum penicillins against Pseudomonas is variable and a wide range of MIC values have been reported for the drugs. In vitro on a weight basis, ticarcillin generally is 2-4 times more active than carbenicillin against Pseudomonas; however, piperacillin generally is more active than a-carboxypenicillins against this organism. In vitro, piperacillin concentrations of 25-32 mcg/mL generally inhibit 75-95% of strains of Ps. aeruginosa tested. Ticarcillin concentrations of 25-64 mcg/mL reportedly inhibit 50-80% of strains of Ps. aeruginosa tested. Carbenicillin concentrations of 25-32 mcg/mL generally inhibit only 39-58% of strains of Ps. aeruginosa tested and concentrations of the drug of 50-64 mcg/mL generally are required to inhibit 65-85% of strains tested. Extended-spectrum penicillins are also active in vitro against Pseudomonas other than Ps. aeruginosa. Piperacillin concentrations of 0.5-16 mcg/mL generally inhibit Ps. putrefaciens, Ps. stutzeri, and Ps. vesicularis in vitro and concentrations of the drug of 1-64 mcg/mL generally inhibit Ps. alcaligenes in vitro. Some strains of these organisms are inhibited in vitro by carbenicillin or ticarcillin concentrations of 1-128 mcg/mL. Ps. fluorescens and Ps. putida generally are resistant to extended-spectrum penicillins.
Other Gram-negative Aerobic Bacilli
Extended-spectrum penicillins are more active than other currently available penicillins against Acinetobacter. Acinetobacter calcoaceticus var. anitratus generally is inhibited in vitro by carbenicillin, piperacillin, or ticarcillin concentrations of 8-64 mcg/mL and A. calcoaceticus var. lwoffi generally is inhibited by concentrations of these drugs of 0.25-64 mcg/mL. Burkholderia cepacia (formerly Pseudomonas cepacia) and Brevundimonas diminuta (formerly Pseudomonas diminuta) generally are inhibited by piperacillin concentrations of 1-64 mcg/mL. Stenotrophomonas maltophilia (formerly Pseudomonas maltophilia) generally is resistant to extended-spectrum penicillin.
Moraxella generally is inhibited in vitro by carbenicillin or ticarcillin concentrations of 0.06-0.5 mcg/mL and piperacillin concentrations of 0.06-8 mcg/mL. Some species of Flavobacterium are inhibited in vitro by piperacillin concentrations of 0.5-64 mcg/mL; most strains of this organism are resistant to carbenicillin and ticarcillin. Extended-spectrum penicillins have some activity against the facultative anaerobe Eikenella corrodens and the MIC90 of piperacillin or ticarcillin reported for this organism is 1-4 mcg/mL.
Pasteurella multocida, an organism that can be aerobic or facultatively anaerobic, is usually inhibited in vitro by carbenicillin or ticarcillin concentrations of 0.1-3 mcg/mL. Extended-spectrum penicillins have some in vitro activity against Legionella, although the drugs may not be effective clinically. In vitro, carbenicillin concentrations of 0.5-4 mcg/mL reportedly inhibit some strains of Legionella pneumophila and carbenicillin concentrations of 0.05-25 mcg/mL inhibit some strains of L. micdadei (the Pittsburgh pneumonia agent) and L. bozemanii.
Carbenicillin concentrations of 0.5-32 mcg/mL inhibit some strains of L. gormanii and L. dumoffii. Carbenicillin reportedly has some activity against Campylobacter fetus, an organism that can be microaerophilic or anaerobic; the MIC90 of the drug reported for some strains of C. fetus subsp. jejuni is 25 mcg/mL. Some strains of Bordetella pertussis reportedly are inhibited by carbenicillin concentrations of 0.25 mcg/mL22 and some strains of Brucella are inhibited in vitro by carbenicillin concentrations of 1.3-12.5 mcg/mL. Gardnerella vaginalis (formerly Haemophilus vaginalis) is inhibited in vitro by carbenicillin concentrations of 0.5 mcg/mL.
Anaerobic Bacteria
Extended-spectrum penicillins generally are less active than aminopenicillins against gram-positive anaerobic bacteria; however, the drugs are active in vitro against some strains of Actinomyces, Bifidobacterium, Clostridium, Eubacterium, Lactobacillus,Peptococcus, Peptostreptococcus, and Propionibacterium. In vitro, C. perfringens and P. acnes generally are inhibited by extended-spectrum penicillin concentrations of 0.1-8 mcg/mL.
Some strains of C. difficile are inhibited in vitro by carbenicillin or piperacillin concentrations of 8 mcg/mL. Extended-spectrum penicillins are also active against gram-negative anaerobes including some strains of Bacteroides, Fusobacterium, Prevotella, and Veillonella. Many strains of Prevotella melaninogenica (formerly B. melaninogenicus) are inhibited in vitro by carbenicillin or ticarcillin concentrations of 0.1-4 mcg/mL.
Extended-spectrum penicillins generally are more active in vitro against the B. fragilis group (e.g., B. fragilis, B. distasonis, B. ovatus, B. thetaiotaomicron, B. vulgatus) than other currently available penicillins. In vitro, some susceptible strains of B. fragilis are inhibited by carbenicillin or ticarcillin concentrations of 16-64 mcg/mL or piperacillin concentrations of 1-32 mcg/mL. Resistance For a discussion of the possible mechanisms of bacterial resistance to penicillins, see Resistance: Mechanisms of Penicillin Resistance, in the Natural Penicillins General Statement 8:12.16.04. Complete cross-resistance generally occurs between carbenicillin and ticarcillin. Cross-resistance among acylaminopenicillins is generally unpredictable.
Resistance in Gram-positive Bacteria
Penicillinase-producing S. aureus and S. epidermidis are resistant to extended-spectrum penicillins because these penicillins generally are inactivated by staphylococcal penicillinases.
Resistance in Gram-negative Bacteria
The majority of penicillinase-producing strains of N. gonorrhoeae are resistant to extended-spectrum penicillins. However, some penicillinase-producing strains of N. gonorrhoeae that are completely resistant to natural penicillins and aminopenicillins may be inhibited in vitro by high concentrations of piperacillin. Some strains of N. gonorrhoeae that are relatively resistant to natural penicillins may also be inhibited in vitro by extended-spectrum penicillins. Although extended-spectrum penicillins are more resistant than natural penicillins, penicillinase-resistant penicillins, and aminopenicillins to inactivation by b-lactamases produced by gram-negative bacteria, the drugs generally are inactivated by Richmond-Sykes type III or TEM-type b-lactamases. Therefore, strains of E. coli, Salmonella, and Shigella that produce these types of b-lactamases are resistant to all currently available extended-spectrum penicillins. Resistance to piperacillin has been reported in 12-50% of clinical isolates of E. coli and resistance to carbenicillin and ticarcillin has been reported in 20-57% of isolates of the organism. Extended-spectrum penicillins generally are rapidly hydrolyzed by b-lactamases produced by Klebsiella. At least 90% of clinical isolates of Klebsiella reportedly are resistant to carbenicillin and ticarcillin; however, less than 10% reportedly are resistant to piperacillin.
Pseudomonas aeruginosa
Resistance to penicillins in Ps. aeruginosa generally results from both the production of a wide variety of b-lactamases and the inability of the drugs to penetrate the outer membrane of the organism. Alterations in the target enzymes (PBPs) have also been identified in some resistant strains of Ps. aeruginosa. Carbenicillin and ticarcillin are hydrolyzed by many b-lactamases produced by Ps. aeruginosa (e.g., PSE 1, 2, 3, and 4). In vitro studies indicate that piperacillin is less stable than carbenicillin or ticarcillin to inactivation by some b-lactamases produced by Ps. aeruginosa; however, piperacillin has greater intrinsic activity against these organisms, presumably because of a greater ability to gain access to the PBPs. Resistant strains of Ps. aeruginosa have developed during therapy with carbenicillin, ticarcillin, or piperacillin.
Approximately 15-35% of clinical isolates of Ps. aeruginosa are resistant to carbenicillin and ticarcillin. However, less than 10% of clinical isolates of Ps. aeruginosa are resistant to piperacillin. Some strains of Ps. aeruginosa resistant to carbenicillin and ticarcillin may be susceptible to piperacillin in vitro. Piperacillin is active in vitro against a few strains of Ps. aeruginosa that are resistant to gentamicin and tobramycin.
Pharmacokinetics
In all studies described in the Pharmacokinetics section, piperacillin was administered as the sodium salt and ticarcillin was administered as the disodium salt; carbenicillin was administered parenterally as the disodium salt (no longer commercially available in the US) and orally as carbenicillin indanyl sodium. Dosages and concentrations of the drugs are expressed in terms of the bases. For more specific information on the pharmacokinetics of carbenicillin and ticarcillin, see Pharmacokinetics in the individual monographs in 8:12.16.04.
Absorption
Piperacillin sodium and ticarcillin disodium are not appreciably absorbed from the GI tract and must be given parenterally. Carbenicillin indanyl sodium is generally stable in the presence of acidic gastric secretions and is rapidly, but incompletely, absorbed following oral administration. For information on absorption of carbenicillin indanyl sodium, see Pharmacokinetics: Absorption, in Carbenicillin Indanyl Sodium 8:12.16.04.
Peak serum concentrations of extended-spectrum penicillins vary with the dose, route, and rate of administration. Acylaminopenicillins (piperacillin) exhibit nonlinear dose-dependent pharmacokinetics, apparently because of capacity-limited saturation of both renal and nonrenal mechanisms for elimination of the drugs. (See Pharmacokinetics: Elimination.)
Peak serum concentrations and areas under the serum concentration-time curves (AUCs) of acylaminopenicillins increase more than proportionally with increases in dosage of the drugs. Although it has been stated that a-carboxypenicillins (carbenicillin, ticarcillin) do not exhibit nonlinear dose-dependent pharmacokinetics, there is some evidence that these drugs also exhibit this effect since their serum half-lives appear to increase slightly with increasing dosage. Piperacillin and ticarcillin are readily absorbed from IM injection sites. Approximately 63% of an IM dose of piperacillin is absorbed from the injection site.
Following IM administration of a single 1- or 2-g dose of piperacillin or ticarcillin in healthy adults, peak serum concentrations of the drugs range from 12.8-63.6 mcg/mL and generally are attained within 30 minutes to 2 hours; serum concentrations of the drugs generally are low or undetectable 6-8 hours later.
Following IV injection over 2-5 minutes of a 2-g dose of piperacillin or ticarcillin in healthy adults, peak serum concentrations immediately following the injection average 199-305 mcg/mL for piperacillin and 200-218 mcg/mL for ticarcillin; serum concentrations of the drugs are low or undetectable 6-8 hours after the injection. In one crossover study in healthy adults who received single 2-g doses of carbenicillin (parenteral formulation no longer commercially available in the US), ticarcillin, and piperacillin infused IV over 30 minutes, peak serum concentrations of the drugs were essentially equal and averaged 53-63. mcg/mL at the end of infusion.
Distribution
Extended-spectrum penicillins are widely distributed following absorption from injection sites.
The volume of distribution of piperacillin reportedly ranges from 0.14-0.31 L/kg in adults and 0.38-0. L/kg in neonates. Carbenicillin and ticarcillin reportedly have volumes of distribution that average 0.34 L/kg in adults and 0.42-0.76 L/kg in neonates. Although results of some studies indicate that the volumes of distribution of acylaminopenicillins generally are unaffected by dosage, studies using piperacillin indicate that volume of distribution of the drug decreases with increasing dosage.
Concomitant administration of probenecid has been reported to increase the volumes of distribution of carbenicillin and ticarcillin, but probenecid appears to decrease the volume of distribution of piperacillin. (See Drug Interactions: Probenecid.) Extended-spectrum penicillins are readily distributed into ascitic, synovial, pleural, peritoneal, and wound fluids. The drugs are also distributed into kidneys, heart, gallbladder, skin, prostate, gynecologic tissues, tonsils, bronchial secretions, muscle, and adipose tissue.
Low concentrations of the drugs are attained in sputum and bone. Concentrations of carbenicillin and ticarcillin in bile may be several times greater than concurrent serum concentrations of the drugs; however, concentrations of acylaminopenicillins in bile generally are 5-300 times greater than concurrent serum concentrations unless biliary obstruction is present.
Like other penicillins, negligible concentrations of extended-spectrum penicillins generally are attained in ocular tissues and fluids following IM or IV administration of the drugs. Only minimal concentrations of extended-spectrum penicillins are attained in CSF following IM or IV administration of the drugs in patients with uninflamed meninges. Higher CSF concentrations may be attained when meninges are inflamed. In one study, CSF concentrations of ticarcillin were 6% of concurrent serum concentrations of the drug in patients with normal meninges and 39% of concurrent serum concentrations in those with inflamed meninges.
Concurrent administration of oral probenecid with IM or IV administration of extended-spectrum penicillins reportedly results in increased CSF concentrations of the drugs. (See Drug Interactions: Probenecid.) The degree of protein binding of extended-spectrum penicillins decreases with increasing concentrations of the drugs. a-Carboxypenicillins generally are more highly protein bound than acylaminopenicillins.
Approximate degrees of protein binding of extended-spectrum penicillins have been reported as follows: Drug % Bound to Serum Proteins carbenicillin 29-60% piperacillin 16-22% ticarcillin 45-65% Results of one in vitro study indicate that carbenicillin is 42-46% bound to human serum proteins at a concentration of 2 mcg/mL, 35-39% bound at a concentration of 20 mcg/mL, and 27-30% bound at a concentration of 200 mcg/mL. Carbenicillin binds mainly to serum albumin. Acylaminopenicillins, unlike most other currently available penicillins, bind to both serum albumin and β-globulin. Piperacillin readily crosses the placenta. Although specific information is not available on distribution of carbenicillin and ticarcillin across the placenta, the drugs probably cross the placenta like other penicillins. Extended-spectrum penicillins are distributed into milk in low concentrations.
Elimination
Serum concentrations of extended-spectrum penicillins decline in a biphasic manner In studies that used various dosages of the drugs in adults with normal renal function, distribution half-lives (t1/2as) and elimination half-lives (t1/2bS) of extended-spectrum penicillins have been reported as follows: t1/2a (in hours) t1/2b (in hours) carbenicillin (none reported) 0.78-1 piperacillin 0.17-0.33 0.6-1.3 ticarcillin 0.1-0.17 0.93-1.3 Acylaminopenicillins exhibit nonlinear dose-dependent pharmacokinetics. The t1/2?s of piperacillin is longer and serum, renal, and nonrenal clearances of the drug decreased with higher dosages than with lower dosages. T
his appears to result from capacity-limited saturation of both renal and nonrenal mechanisms for elimination of the drug. Piperacillin reportedly has a t1/2b of 0.6 hours after a single 1-g dose of the drug, 0.72 hours after a single 2-g dose, and 1.05 hours after a single 6-g dose. Although there is little published information on the relationship of dosage and pharmacokinetics of a-carboxypenicillins and it has been stated that these drugs do not exhibit nonlinear dose-dependent pharmacokinetics, the serum half-lives of carbenicillin and ticarcillin also appear to increase slightly with increasing dosage. Extended-spectrum penicillins are metabolized to varying extents.
Following oral administration, carbenicillin indanyl sodium is rapidly hydrolyzed by plasma and tissue esterases to carbenicillin and indanol; indanol is rapidly excreted in urine as glucuronide and sulfate conjugates. Approximately 10-15% of a single IM or IV dose of ticarcillin is metabolized by hydrolysis of the b-lactam ring to penicilloic acids which are microbiologically inactive. In one study, an unidentified active metabolite of carbenicillin and ticarcillin was also found in urine.
Although the metabolic fate of piperacillin has not been elucidated to date, the drug does not appear to be metabolized to any appreciable extent. Extended-spectrum penicillins and their metabolites are rapidly excreted principally in urine by tubular secretion and glomerular filtration. The drugs are also partly excreted via bile, but biliary elimination is decreased in patients with biliary obstruction. Following IV administration of single 1- or 2-g doses of the drugs in adults with normal renal function, approximately 42-90% of the piperacillin dose and 80-93% of the ticarcillin dose are excreted unchanged in urine within 24 hours.
As with other penicillins, most of the dose is excreted during the first 2-6 hours. In patients with normal renal and hepatic function, 10-20% of a single dose of piperacillin is excreted via bile. Serum clearance of piperacillin reportedly ranges from 153-297 mL/minute per 1.73 m in adults with normal renal and hepatic function. Carbenicillin reportedly has a serum clearance of 125-132 mL/minute and ticarcillin has a serum clearance of 132-253 mL/minute in adults with normal renal and hepatic function. Serum concentrations of extended-spectrum penicillins are higher and serum half-lives are prolonged in patients with impaired renal function.Nonlinear dose-dependent pharmacokinetics of acylaminopenicillins are more pronounced in patients with renal impairment than in patients with normal renal function.
The serum half-lives of carbenicillin and ticarcillin in patients with renal impairment are prolonged to a greater extent than are the serum half-lives of acylaminopenicillins. In patients with creatinine clearances less than 10 mL/minute per 1.73 m, the t1/2b of piperacillin reportedly ranged from 2.1-14 hours. The serum half-life of carbenicillin reportedly ranges from 9.4-23. hours in patients with creatinine clearances less than 10 mL/minute per 1.73 m and the serum half-life of ticarcillin in these patients reportedly ranges from 13.5-16.2 hours. Hepatic impairment also increases serum concentrations of extended-spectrum penicillins and prolongs the serum half-lives of the drugs. In patients with both renal and hepatic impairment, the serum half-lives of carbenicillin, piperacillin, and ticarcillin reportedly may range up to 32 hours.
Serum concentrations of extended-spectrum penicillins generally are higher and the serum half-lives of the drugs are longer in neonates than in older children and adults because of immature mechanisms for tubular secretion. The serum half-lives of carbenicillin, piperacillin, and ticarcillin reportedly range from 1.8-6.7 hours in neonates depending on age and weight. Studies using carbenicillin and ticarcillin indicate that the serum half-lives of the drugs generally are inversely proportional to birthweight, gestational age, and chronologic age. Oral probenecid administered shortly before or with an extended-spectrum penicillin competitively inhibits renal tubular secretion of the penicillin and produces higher and prolonged serum concentrations of the drug. (See Drug Interactions: Probenecid.)
Studies using piperacillin and ticarcillin indicate that patients with cystic fibrosis eliminate these drugs at a faster rate than do healthy individuals, presumably because of increased tubular secretion. This effect may be clinically important since use of usual dosages of extended-spectrum penicillins in cystic fibrosis patients may result in lower serum concentrations of the drugs than expected. Carbenicillin, piperacillin, and ticarcillin are removed by hemodialysis. The amount of the drugs removed during hemodialysis depends on several factors (e.g., type of coil used, dialysis flow-rate); however, a 4- to 6-hour period of hemodialysis reportedly removes into the dialysate 6-50% of a single IV or IM dose of piperacillin. Small amounts of carbenicillin, piperacillin, and ticarcillin are removed by peritoneal dialysis.
Chemistry and Stability
Chemistry
Extended-spectrum penicillins are a group of semisynthetic penicillin derivatives that, because of their chemical structures, have wider spectra of activity than natural penicillins, penicillinase-resistant penicillins, and aminopenicillins. The extended spectrum penicillins group is composed of 2 different subgroups: a-CARBOXYPENICILLINS carbenicillin ticarcillin ACYLAMINOPENICILLINS piperacillin a-Carboxypenicillins have a carboxylic acid group at the a-position at R on the penicillin nucleus which results in activity against some strains of Pseudomonas and stability against b-lactamases produced by Proteus.
Acylaminopenicillins have a basic group on the side chain at R on the penicillin nucleus which generally results in even greater activity against Pseudomonas and Enterobacteriaceae compared with a-carboxypenicillins. (For information on the penicillin nucleus, see the Preface to the General Statements on Penicillins 8:12.16.) Carbenicillin differs structurally from ampicillin only in the substitution of an a-carboxy group for the a-amino group on the side chain of the penicillin nucleus. Ticarcillin is the 3-thienyl analog of carbenicillin. Piperacillin is a piperazine derivative of ampicillin.
Carbenicillin is commercially available as the sodium salt of its indanyl ester; carbenicillin indanyl sodium is rapidly hydrolyzed to carbenicillin in vivo. Ticarcillin is commercially available as the disodium salt. Ticarcillin disodium is available alone and also is commercially available in a fixed-ratio combination with clavulanate potassium. Piperacillin is commercially available in the US only as the sodium salt in fixed-combination with tazobactam as the sodium salt. Potency of the sodium or disodium salts of extended-spectrum penicillins is expressed in terms of their bases; potency of carbenicillin indanyl sodium is expressed in terms of carbenicillin. Extended-spectrum penicillins generally are soluble to freely soluble in water and slightly soluble to soluble in alcohol.
Stability
Extended-spectrum penicillins generally are stable for several years in the dry state at room temperature; however, the drugs are stable only for short periods of time in solution unless frozen. Like other penicillins, stability of extended-spectrum penicillins is pH and temperature dependent. The drugs generally are stable at pH 4.5-8.5. Piperacillin sodium and ticarcillin disodium are unstable in acid.
Ticarcillin reportedly has a half-life of 45 minutes or less in solutions with a pH of 2 at 37°C. Esterification of the a-carboxy group helps prevent decarboxylation of carbenicillin; therefore, carbenicillin indanyl sodium is more resistant to acid-catalyzed hydrolysis than carbenicillin and is generally stable in the presence of acidic gastric secretions following oral administration. Extended-spectrum penicillins are hygroscopic, and dry powders of the drugs should be protected from moisture to prevent hydrolysis. Piperacillin sodium and solutions of the drug may darken on exposure to sunlight; however, discoloration does not indicate loss of potency.
Small amounts of polymer conjugation products reportedly form in solutions of ticarcillin disodium during in vitro storage, especially when high concentrations of the drug are stored at room temperature. Because these polymers may play a role in hypersensitivity reactions to penicillins, some clinicians suggest that, although potency may not be adversely affected, solutions of the drug should generally be refrigerated or used within a short time following preparation. For a discussion of the role of penicillin degradation products in sensitization to penicillins, see Cautions: Hypersensitivity Reactions, in the Natural Penicillins General Statement 8:12.16.04.
Like other penicillins, extended-spectrum penicillins are potentially physically and/or chemically incompatible with some drugs, including aminoglycosides, but the compatibility depends on the specific drug and several other factors (e.g., concentration of the drugs, specific diluents used, resulting pH, temperature). For information on the in vitro and in vivo incompatibility of penicillins and aminoglycosides, see Drug Interactions: Aminoglycosides. For a more complete discussion of the stability of ticarcillin and solutions of the drugs, see Chemistry and Stability: Stability, in the individual monograph in 8:12.16.16. For specific information on dosage and administration and additional information on chemistry and stability and pharmacokinetics, see the individual monographs on Carbenicillin Indanyl Sodium, and Ticarcillin Disodium in 8:12.16.16.




