Ertapenem is a synthetic carbapenem b-lactam antibiotic that is structurally and pharmacologically related to imipenem and meropenem. Like meropenem but unlike imipenem, ertapenem has a methyl group at position 1 of the 5-membered ring, which confers stability against hydrolysis by dehydropeptidase 1 (DHP 1) present on the brush border of proximal renal tubular cells, and therefore does not require concomitant administration with a DHP-1 inhibitor such as cilastatin. Ertapenem is almost completely absorbed following IM administration, having a mean bioavailability of 90%.
Ertapenem exhibits nonlinear pharmacokinetics and is highly bound to plasma proteins, principally albumin. The drug has a mean plasma half-life of approximately 4 hours and may be administered once daily. (See Dosage and Administration: General Dosage.) Ertapenem does not inhibit cytochrome P-450 (CYP) isoenzymes 1A2, 2C9, 2C19, 2D6, 2E1, or 3A4 in vitro and does not inhibit the p-glycoprotein transport system or act as a substrate for p-glycoprotein-mediated transport.(See Drug Interactions: Drugs with p-Glycoprotein-Mediated Clearance.) The drug is eliminated principally by renal excretion.
Ertapenem has in vitro activity against gram-positive and gram-negative aerobic and anaerobic bacteria. The drug is stable in the presence of a variety of b-lactamases (including penicillinases, cephalosporinases, and extended-spectrum b-lactamases).
Ertapenem is active in vitro and in clinical infections against most strains of Staphylococcus aureus (methicillin-susceptible strains only), Streptococcus agalactiae, S. pneumoniae (penicillin-susceptible strains only), S. pyogenes, Escherichia coli, Haemophilus influenzae (non-b-lactamase-producing strains only), Klebsiella pneumoniae, Moraxella catarrhalis, Bacteroides fragilis, B. distasonis, B. ovatus, B. thetaiotaomicron, B. uniformis, Clostridium clostridioforme, Eubacterium lentum, Peptostreptococcus spp., Porphyromonas asaccharolytica, and Prevotella bivia. Ertapenem also has demonstrated in vitro activity against S. pneumoniae (penicillin-intermediate strains), Citrobacter freundii, C. koseri, Enterobacter aerogenes, E. cloacae, H. influenzae (b-lactamase-producing strains), H. parainfluenzae, Klebsiella oxytoca (excluding extended-spectrum b-lactamase-producing strains), Morganella morganii, Proteus mirabilis, P. vulgaris, Serratia marcescens, C. perfringens, and Fusobacterium spp.; however, the safety and efficacy of ertapenem in treating clinical infections caused by these microorganisms have not been established in adequate and well-controlled clinical trials to date. Each gram of ertapenem provides approximately 6 mEq (137 mg) of sodium.
Uses
Ertapenem is used IV in adults for the treatment of moderate to severe infections, including complicated intra-abdominal and acute pelvic infections, complicated skin and skin structure infections, community-acquired pneumonia, and complicated urinary tract infections, caused by susceptible organisms.
Intra-abdominal and Gynecologic Infections
Ertapenem is used IV for the treatment of complicated intra-abdominal infections caused by susceptible strains of Escherichia coli, Clostridium clostridioforme (C. clostridiiforme), Eubacterium lentum, Peptostreptococcus spp., Bacteroides fragilis, B. distasonis, B. ovatus, B. thetaiotaomicron, or B. uniformis. In a clinical trial in patients with complicated intra-abdominal infections, the combined clinical and microbiologic cure rate at 4-6 weeks following treatment was 84 or 80% in patients receiving ertapenem (1 g IV daily) or piperacillin sodium and tazobactam sodium (3.375 g [3 g of piperacillin and 0.375 g of tazobactam] IV every 6 hours), respectively, for 5-14 days.
Ertapenem is used IV for the treatment of acute pelvic infections, including postpartum endomyometritis, septic abortion, and postsurgical gynecologic infections, caused by susceptible strains of Streptococcus agalactiae, E. coli, B. fragilis, Porphyromonas asaccharolytica (B. asaccharolytica), Peptostreptococcus spp., or Prevotella bivia. Clinical success at 2-4 weeks following treatment was achieved in 94% of patients receiving ertapenem (1 g IV daily) and 92% of those receiving piperacillin sodium and tazobactam sodium (3. g [3 g of piperacillin and 0.375 g of tazobactam] IV every 6 hours) for 3-10 days.
Skin and Skin Structure Infections
Ertapenem is used IV for the treatment of complicated skin and skin structure infections caused by susceptible strains of Staphylococcus aureus (methicillin-susceptible strains only), Streptococcus pyogenes, E. coli, or Peptostreptococcus spp. In a clinical trial in patients with complicated skin and skin structure infections, clinical success at 10-21 days following treatment was achieved in 84% of patients receiving ertapenem (1 g IV daily) and 85% of those receiving piperacillin sodium and tazobactam sodium (3.375 g [3 g of piperacillin and 0.375 g of tazobactam] IV every 6 hours) for 7-14 days.
Community-acquired Pneumonia
Ertapenem is used IV for the treatment of community-acquired pneumonia caused by susceptible strains of Streptococcus pneumoniae (penicillin-susceptible strains only), including cases with concurrent bacteremia, Haemophilus influenzae (non-b-lactamase-producing strains only), or Moraxella (formerly Branhamella) catarrhalis. In 2 clinical trials, clinical success rates at 7-14 days following treatment were similar (91-92%) with ertapenem (1 g IV daily) and with ceftriaxone (1 g IV daily). Anti-infective therapy was continued for 10-14 days; each regimen included an option to switch to oral amoxicillin trihydrate and clavulanate potassium to complete the course of therapy.
Urinary Tract Infections
Ertapenem is used IV for the treatment of complicated urinary tract infections, including pyelonephritis, caused by susceptible strains of E. coli, including cases with concurrent bacteremia, or Klebsiella pneumoniae. Pooled data from 2 clinical trials in patients with complicated urinary tract infections showed a microbiologic cure rate at 5-9 days following treatment of 90 or 91% in patients receiving ertapenem (1 g IV daily) or ceftriaxone (1 g IV daily), respectively. Anti-infective therapy was continued for 10-14 days; each regimen included an option to switch to oral ciprofloxacin to complete the course of therapy.
Dosage and Administration
Reconstitution and Administration
Ertapenem sodium is administered by IV infusion over 30 minutes or by IM injection. The manufacturer states that the drug may be administered once daily by IV infusion for up to 14 days or by IM injection for up to 7 days. For IV infusion, ertapenem sodium powder for injection must be reconstituted and diluted prior to administration.
The manufacturer states that 10 mL of sterile water for injection, 0.9% sodium chloride injection, or bacteriostatic water for injection should be used to reconstitute the powder and then the reconstituted solution should be further diluted with 50 mL of 0.9% sodium chloride. The reconstituted solution may be stored at room temperature and infused IV within 6 hours of reconstitution or refrigerated at 5°C for up to 24 hours and infused IV within 4 hours after removal from the refrigerator.
Solutions of ertapenem sodium should not be frozen. Ertapenem sodium shouldnot be reconstituted or diluted with dextrose-containing solutions or admixed with other drugs. For IM injection, ertapenem sodium powder for injection must be reconstituted with 3.2 mL of 1% lidocaine injection (without epinephrine) and shaken thoroughly to ensure dissolution; this solution should not be administered IV. The entire contents of the vial should be withdrawn, and injected IM deeply into a large muscle mass, such as the gluteus or lateral part of the thigh.
Parenteral ertapenem sodium solutions should be inspected visually for particulate matter and discoloration prior to administration whenever solution and container permit.
Dosage
Dosage of ertapenem sodium is expressed in terms of ertapenem. The usual adult dosage of ertapenem is 1 g once daily. The duration of ertapenem therapy depends on the type and severity of infection.
The manufacturer recommends that anti-infective therapy generally be continued for 5-14 days in patients with complicated intra-abdominal infections, 7-14 days in patients with complicated skin and skin structure infections, 10-14 days in patients with community-acquired pneumonia or complicated urinary tract infections (including pyelonephritis), and 3-10 days in patients with acute pelvic infections including postpartum endomyometritis, septic abortion, and postsurgical gynecologic infections. Patients with community-acquired pneumonia or complicated urinary tract infections who are treated initially with IV ertapenem may be switched to oral therapy after at least 3 days of parenteral therapy, if clinically appropriate.
Special Populations
No dosage adjustment is necessary in adults with creatinine clearances exceeding 30 mL/minute per 1.73 m; however, the manufacturer recommends a dosage of 500 mg daily for those with severe renal impairment (creatinine clearance of 30 mL/minute per 1.73 m or less) or end-stage renal disease (creatinine clearance of 10 mL/minute per 1.73 m or less). In adults undergoing hemodialysis, the manufacturer also recommends a dosage of 500 mg daily. If the daily dose is given within 6 hours prior to hemodialysis, a supplemental dose of 150 mg should be administered following the dialysis period; a supplemental dose is not necessary if the daily dose is given at least 6 hours prior to hemodialysis.
Cautions
Contraindications
Known hypersensitivity to ertapenem, other carbapenems, or any ingredient in the formulation; history of anaphylactic reaction to b-lactams. Patients with known hypersensitivity to local anesthetics of the amide type should not receive ertapenem sodium reconstituted with lidocaine hydrochloride for IM injection.
Warnings/Precautions
Sensitivity Reactions Hypersensitivity Reactions Serious and occasionally fatal hypersensitivity reactions have been reported in patients receiving b-lactams. Ertapenem should be discontinued at the first appearance of a rash or any other sign of hypersensitivity. Major Toxicities Clostridium difficile-associated Colitis Reported with numerous anti-infectives, including ertapenem; may range in severity from mild to life-threatening.
Evaluate and monitor patients who develop diarrhea during therapy. General Precautions Seizures Reported in patients receiving ertapenem. Caution is advised in patients with known or suspected CNS disorders (e.g., brain lesions, history of seizures) or compromised renal function. Specific Populations Pregnancy Category B. (See Users Guide.) Lactation Ertapenem is distributed into breast milk; caution if used in nursing women. Pediatric Use Safety and efficacy not established in children younger than 18 years of age. Geriatric Use No substantial differences in safety and efficacy relative to younger adults.
Common Adverse Effects
Adverse effects occurring in 1% or more of patients receiving ertapenem sodium include diarrhea, infused vein complication, nausea, headache, vaginitis, phlebitis or thrombophlebitis, and vomiting.
Drug Interactions
Probenecid
Pharmacokinetic interaction (decreased clearance of ertapenem). Concomitant use of probenecid to prolong the half-life of ertapenem is not recommended.
Drugs Metabolized by Hepatic Microsomal Enzymes
Pharmacokinetic interaction unlikely.
Drugs with p-Glycoprotein-mediated Clearance
Pharmacokinetic interaction unlikely for drugs that undergo p-glycoprotein-mediated clearance (e.g., digoxin, vinblastine).
Advice to Patients
Importance of informing clinicians of other medical conditions, including any history of seizures. Importance of monitoring for signs of hypersensitivity reaction. Importance of reporting persistent or worsening symptoms of infection. Importance of women informing clinicians if they are or plan to become pregnant or to breast-feed. Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs. Overview® (see Users Guide). For additional information on this drug until a more detailed monograph is developed and published, the manufacturer’s labeling should be consulted. It is essential that the manufacturer’s labeling be consulted for more detailed information on usual cautions, precautions, contraindications, potential drug interactions, laboratory test interferences, and acute toxicity.
Preparations
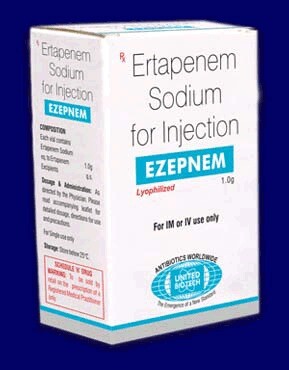
Ertapenem Sodium Parenteral For injection 1 g (of ertapenem) Invanz®, Merck

