Cefotetan is a semisynthetic cephamycin b-lactam antibiotic.
Uses
Cefotetan is used for the treatment of urinary tract, lower respiratory tract, skin and skin structure, bone and joint, gynecologic, and intra-abdominal infections caused by susceptible bacteria and is used for perioperative prophylaxis.
Cefotetan should not be used in the treatment of meningitis or other CNS infections. Prior to initiation of cefotetan therapy, appropriate specimens should be obtained for identification of the causative organism and in vitro susceptibility tests.
Cefotetan therapy may be started pending results of susceptibility tests, but should be discontinued if the organism is found to be resistant to the drug. In certain serious infections, including confirmed or suspected gram-positive or gram-negative sepsis, when the causative organism is unknown, cefotetan and concomitant therapy with an aminoglycoside may be indicated initially pending results of susceptibility tests. If an aminoglycoside is used concomitantly with cefotetan, renal function should be monitored, especially if high aminoglycoside dosage is used or if concomitant therapy is prolonged.
Gram-positive Aerobic Bacterial Infections
Cefotetan is used in adults for the treatment of lower respiratory tract infections caused by susceptible Streptococcus pneumoniae or Staphylococcus aureus; gynecologic or skin or skin structure infections caused by susceptible S. aureus, S. epidermidis, streptococci or group B streptococci; and intra-abdominal infections caused by susceptible streptococci. The drug also has been used effectively in a limited number of adults for the treatment of bone and joint infections caused by susceptibleS. aureus or urinary tract infections caused by susceptible S. aureus or S epidermidis. Cefotetan, like second and third generation cephalosporins, generally is not a drug of choice for the treatment of infections caused by gram-positive bacteria and should not be used in the treatment of infections caused by these organisms when a penicillin or a first generation cephalosporin could be used.
Gram-negative Aerobic Bacterial Infections
Cefotetan is used in adults for the treatment of urinary tract infections caused by susceptible Escherichia coli, Klebsiella, Proteus mirabilis, P. vulgaris, Providencia rettgeri, or Morganella morganii; lower respiratory tract infections caused by susceptible Haemophilus influenzae, E. coli, P. mirabilis, Serratia marcescens, or Klebsiella; and skin and skin structure infections caused by susceptible E. coli or K. pneumoniae. The drug is also used in adults for the treatment of intra-abdominal infections caused by susceptible E. coli or Klebsiella or gynecologic infections caused by susceptible E. coli, P. mirabilis, or N. gonorrhoeae. Cefotetan generally has been as effective as cefoxitin or cefotaxime in the treatment of urinary tract infections caused by susceptible gram-negative bacteria. Because Pseudomonas aeruginosa generally are resistant to cefotetan, the drug should not be used in the treatment of any infection where Ps. aeruginosa may be the causative organism.
Anaerobic and Mixed Aerobic-Anaerobic Bacterial Infections
Cefotetan is used in the treatment of gynecologic infections caused by susceptible gram-positive anaerobic cocci, including Peptococcus and Peptostreptococcus, or susceptible Fusobacterium and skin and skin structure infections caused by Peptococcus and Peptostreptococcus. The drug also is used in the treatment of gynecologic and intra-abdominal infections caused by susceptible Bacteroides or Clostridium. Cefotetan has been used effectively for the treatment of mild to moderate infections caused by B. fragilis, but other anti-infectives (e.g., metronidazole, clindamycin) are preferred for the treatment of severe or life-threatening B. fragilis infections. Cefotetan generally has been effective when used in the treatment of mixed aerobic-anaerobic bacterial infections, including peritonitis and gynecologic infections (see Uses: Pelvic Inflammatory Disease). The drug is unlikely to be effective in the treatment of infections caused by B. distasonis, B. ovatus, or B. thetaiotaomicron since these organisms generally are resistant to the drug.
Pelvic Inflammatory Disease
Cefotetan is used for the treatment of pelvic inflammatory disease (PID) caused by N. gonorrhoeae. Cefotetan, like cephalosporins, generally is inactive against C. trachomatis and should not be used alone in the treatment of PID. PID is an acute or chronic inflammatory disorder in the upper female genital tract and can include any combination of endometritis, salpingitis, tubo-ovarian abscess, and pelvic peritonitis. PID generally is a polymicrobial infection most frequently caused by N. gonorrhoeae and/or Chlamydia trachomatis; however, organisms that can be part of the normal vaginal flora (e.g., anaerobic bacteria, Gardnerella vaginalis, H. influenzae, enteric gram-negative bacilli, S. agalactiae) or mycoplasma (e.g., Mycoplasma hominis, Ureaplasma urealyticum) also may be involved. PID is treated with an empiric regimen that provides broad spectrum coverage.
The regimen should be effective against N. gonorrhoeae and C. trachomatis and also probably should be effective against anaerobes, gram-negative facultative bacteria, and streptococci. The optimum empiric regimen for the treatment of PID has not been identified.
A wide variety of parenteral and oral regimens have been shown to achieve clinical and microbiologic cure in randomized studies with short-term follow-up; however, only limited data are available to date regarding elimination of infection in the endometrium and fallopian tubes or intermediate or long-term outcomes, including the impact of these regimens on the incidence of long-term sequelae of PID (e.g., tubal infertility, ectopic pregnancy, pain) is unknown.
Although many clinicians previously recommended that all patients with acute PID be hospitalized so that adequate bed rest and supervised treatment with parenteral anti-infectives could be initiated, the US Centers for Disease Control and Prevention (CDC) currently states that decisions regarding the necessity for hospitalization and whether an oral or parenteral regimen are most appropriate should be made on an individual basis pending accumulation of data from ongoing studies comparing efficacy of parenteral inpatient therapy and oral outpatient therapy for women with mild PID.
Based on observational data and theoretical concerns, the CDC states that hospitalization is indicated if surgical emergencies such as appendicitis cannot be excluded; the patient is pregnant; the patient is unable to follow or tolerate an outpatient oral regimen; the patient has severe illness, nausea and vomiting, or high fever; the patient has a tuboovarian abscess; the patient is immunodeficient because of HIV infection, immunosuppressive therapy, or other disease; or a clinical response was not obtained with an oral anti-infective regimen.
Parenteral Regimens for PID
When a parenteral regimen is indicated for the treatment of patients with PID, the CDC and other clinicians generally recommend a 2-drug regimen of cefotetan (2 g IV every 12 hours) or cefoxitin (2 g IV every 6 hours) given in conjunction with doxycycline (100 mg IV or orally every 12 hours) or a 2-drug regimen of clindamycin (900 mg IV every 8 hours) and gentamicin (usually a 2-mg/kg IV or IM loading dose followed by 1.5 mg/kg every 8 hours). While there is some evidence that parenteral cephalosporins (e.g., ceftizoxime, cefotaxime, ceftriaxone) also may be effective for the treatment of PID, the CDC states that there is less experience with use of these cephalosporins in patients with PID and these drugs may be less active than cefotetan or cefoxitin against anaerobic bacteria.
Traditionally, parenteral regimens for the treatment of PID have been continued for at least 48 hours after the patient demonstrates substantial clinical improvement and then an oral regimen is continued to complete a total of 14 days of therapy; however, the CDC states that a transition to oral therapy may occur within 24 hours after the patient demonstrates clinical improvement and that decisions regarding such a transition should be guided by clinical experience. Most clinicians recommend at least 24 hours of direct inpatient observation for patients with tubo-ovarian abscesses, after which time anti-infective therapy at home is adequate.
Oral Regimens for PID
When PID is treated with an oral regimen, the CDC and other clinicians generally recommend a 14-day regimen that consists of oral ofloxacin (400 mg twice daily) or oral levofloxacin (500 mg once daily) with or without oral metronidazole (500 mg twice daily for 14 days) or a regimen that consists of a single dose of cefoxitin or a parenteral cephalosporin (e.g., ceftriaxone, ceftizoxime, cefotaxime) given in conjunction with a 14-day regimen of oral doxycycline with or without oral metronidazole (500 mg twice daily for 14 days). Although ofloxacin is effective against both N. gonorrhoeae and C. trachomatis, the addition of metronidazole to the fluoroquinolone regimen may be necessary to provide adequate coverage against anaerobes.
The optimal parenteral cephalosporin or cephamycin for this outpatient regimen is unclear; however, cefoxitin or ceftriaxone usually is preferred. There is evidence from clinical trials that a single 2-g IM dose of cefoxitin (given with a single 1-g oral dose of probenecid) effectively produces a short-term clinical response in women with PID; however, because of theoretical limitations in cefoxitin’s coverage of anaerobes, the addition of metronidazole to the regimen is necessary. In addition, metronidazole should be effective in the treatment of bacterial vaginosis, which is frequently associated with PID.
There are some data suggesting that use of oral doxycycline and oral metronidazole after primary parenteral therapy is safe and effective.
Patient Follow-up and Management of Sexual Partners
Regardless of whether an oral or parenteral regimen is used, patients with PID should demonstrate substantial clinical improvement (e.g., defervescence; reduction in direct or rebound abdominal tenderness; reduction in uterine, adnexal, and cervical motion tenderness) within 72 hours after initiation of anti-infective therapy, and patients being treated on an outpatient basis should receive a follow-up examination within this period to ensure that a response is obtained. Patients who do not respond to therapy within 72 hours usually require hospitalization, additional diagnostic tests, and surgical intervention. In women who had documented infections with N. gonorrhoeae or C. trachomatis, some experts recommend rescreening for these organisms 4-6 weeks after therapy is completed.
Sexual partners of women with PID should be examined and treated if they had sexual contact during the 60 days preceding the onset of symptoms in the patients. Evaluation and treatment are imperative because of the risk for reinfection and the strong likelihood of urethral gonococcal or chlamydial infection in the partner. Male partners of women with PID caused by N. gonorrhoeae or C. trachomatis often are asymptomatic. Sex partners should be treated empirically with regimens effective against these organisms, regardless of the apparent etiology of PID or pathogens isolated from the infected woman.
Gonorrhea and Associated Infections
Cefotetan (a single 1-g IM dose) has been used for the treatment of uncomplicated gonorrhea in adults. However, cefotetan is not included in current CDC recommendations for the treatment of gonococcal infections. For information on current recommendations regarding the treatment of gonorrhea and associated infections, see Uses: Gonorrhea and Associated Infections in Ceftriaxone 8:12.06..
Perioperative Prophylaxis
Cefotetan has been effective when used perioperatively to reduce the incidence of infection in patients undergoing cesarean section, abdominal or vaginal hysterectomy, or transurethral, biliary tract, or GI surgery. There is evidence that perioperative prophylaxis with an appropriate anti-infective agent can decrease the incidence of infection, particularly wound infection, after certain procedures; however, the benefits of prophylaxis must be weighed against the risks of adverse effects (including sensitivity reactions), emergence of resistant bacteria or superinfection, drug interactions, and cost. Therefore, such prophylaxis usually is recommended only for procedures with a high rate of infection, procedures involving implantation of prosthetic material, and procedures in which the consequences of infection are especially serious.
Gynecologic and Obstetric Surgery
Perioperative prophylaxis decreases the incidence of infection after vaginal or abdominal hysterectomy. In addition, perioperative prophylaxis can prevent infection after emergency cesarean section in high-risk situations (e.g., active labor or premature rupture of membranes), after second trimester abortions, or after first trimester abortion in high-risk women. A pooled analysis of results of randomized, placebo-controlled studies in women who underwent therapeutic abortion before 16 weeks’ gestation indicates that perioperative prophylaxis can reduce the overall risk of postabortal infection in these women by 42% compared with placebo.
Some clinicians suggest that the preferred agents for perioperative prophylaxis in women undergoing vaginal or abdominal hysterectomy are IV cefazolin, IV cefotetan, or IV cefoxitin; IV cefazolin generally is the preferred agent for prophylaxis in women undergoing high-risk cesarean section or second trimester abortion; and IV penicillin G or oral doxycycline is preferred for high-risk first trimester abortions (previous history of PID or gonorrhea, multiple sexual partners). In a limited number of patients, a single dose of cefotetan appeared to be at least as effective as multiple doses of cefoxitin for perioperative prophylaxis in patients undergoing vaginal or abdominal hysterectomy and at least as effective as multiple doses of cefoxitin or cefazolin in patients undergoing cesarean section.
Results of a prospective, randomized study indicate that single-dose regimens of cefazolin, cefotetan, or ampicillin sodium and sulbactam sodium are equally effective in decreasing the incidence of postpartum infections in women undergoing high-risk cesarean section; postpartum endomyometritis was reported in 14.3% of those who received cefazolin, 11.1% of those who received cefotetan, and 7.4% of those who received ampicillin sodium and sulbactam sodium.
GI Surgery
There is evidence that perioperative prophylaxis can decrease the incidence of infection after colorectal surgery, and such prophylaxis usually is recommended. For perioperative prophylaxis in patients undergoing colorectal surgery, some clinicians recommend a regimen of IV cefotetan or IV cefoxitin; a regimen of IV cefazolin and IV metronidazole; or a regimen of oral erythromycin and oral neomycin.
It has been suggested that the oral regimen may be as effective as the parenteral regimens. Many clinicians use both the oral regimen and a parenteral regimen for perioperative prophylaxis in patients undergoing colorectal surgery; however, it is unclear whether this combined regimen is more effective than use of either an oral or parenteral regimen alone. In a randomized, prospective study in patients undergoing elective colorectal surgery, the overall incidence of intra-abdominal septic complications in those who received mechanical bowel preparation and an oral regimen (erythromycin and neomycin) alone was similar to that in those who received both the oral regimen and a parenteral regimen (cefoxitin); however, the incidence of abdominal wound infection was higher in those who received the oral regimen alone (14.%) than in those who received the combined oral and parenteral regimen (5%). T
here is evidence that perioperative prophylaxis can reduce the incidence of infection after surgery for acute appendicitis, and some clinicians recommend use of IV cefotetan or IV cefoxitin for perioperative prophylaxis in patients undergoing nonperforated appendectomy. If perforation has occurred, anti-infectives are considered treatment rather than prophylaxis and are continued postoperatively for several days. (See Contaminated Surgery under Uses: Perioperative Prophylaxis.)
For perioperative prophylaxis in high-risk patients undergoing esophageal or gastroduodenal surgery (e.g., those who are morbidly obese or have esophageal obstruction, decreased gastric acidity, or decreased GI motility) or high-risk patients undergoing biliary tract surgery (e.g., those older than 70 years of age or those with acute cholecystitis, nonfunctioning gallbladder, obstructive jaundice, or common duct stones), many clinicians recommend IV cefazolin as the drug of choice; however, some clinicians prefer cefoxitin in patients undergoing these procedures since it provides better coverage against anaerobic bacteria. Results of controlled studies indicate that a single dose of cefotetan is at least as effective as a single dose of cefazolin in reducing the incidence of infection in patients undergoing upper GI69 or biliary tract surgery. A single dose of cefotetan has also been as effective as multiple doses of cefoxitin for perioperative prophylaxis in patients undergoing colorectal surgery and as effective as multiple doses of cefotaxime for perioperative prophylaxis in patients undergoing transurethral surgery.
Timing and Number of Doses
When perioperative prophylaxis is indicated in patients undergoing clean-contaminated or potentially contaminated surgery, administration of the anti-infective should be timed to ensure that bactericidal concentrations of the drug are established in serum and tissues by the time the initial surgical incision is made; therapeutic concentrations of the drug should then be maintained in serum and tissues throughout the operation and until, at most, a few hours after the incision is closed.
With many anti-infectives (e.g., cefazolin), a single dose given no more than 30 minutes before the incision provides adequate tissue concentrations throughout the procedure. If cefotetan is used prophylactically, the manufacturer recommends that the drug be given just prior to surgery (approximately 30-60 minutes before the initial incision) to ensure adequate cefotetan tissue concentrations at the time of surgery.
If surgery is prolonged (more than 4 hours), major blood loss occurs, or an anti-infective with a short half-life (e.g., cefoxitin) is used, it may be advisable to administer one or more additional doses during the procedure; some clinicians suggest that intraoperative doses be administered every 4-8 hours for the duration of the procedure. Although anti-infective prophylaxis regimens reported in published studies often include 1 or 2 postoperative doses, many clinicians state that postoperative doses generally are unnecessary. Continuation of prophylaxis after surgery appears to be of no additional value and may increase the risk of toxicity and bacterial superinfection. If signs of infection occur following surgery, specimens should be obtained for identification of the causative organism and appropriate therapy instituted.
Contaminated Surgery
Patients undergoing contaminated or dirty surgery, such as that involving a perforated abdominal viscus, a compound fracture, a traumatic wound, or a laceration due to an animal or human bite are at risk for infection. When used in patients undergoing these procedures, anti-infective therapy is considered treatment rather than prophylaxis and is continued postoperatively for about 5 days. Some clinicians recommend use of a regimen of IV cefotetan or IV cefoxitin (with or without IV gentamicin) or, alternatively, a regimen of IV clindamycin and IV gentamicin for patients undergoing surgery involving a ruptured viscus; if ruptured viscus occurs in a postoperative setting (dehiscence), anti-infective coverage of nosocomial pathogens should be included. Cefazolin generally is the preferred anti-infective in patients undergoing surgery involving a traumatic wound; some clinicians state that if a bitewound is involved, an anti-infective against anaerobes (e.g., amoxicillin and clavulanate potassium or ampicillin sodium and sulbactam sodium) should be used. For penetrating intracranial wounds, including gunshot injuries, a broad-spectrum anti-infective such as ampicillin sodium and sulbactam sodium is recommended.
Dosage and Administration
Reconstitution and Administration
Cefotetan disodium is administered by IV injection or infusion or by deep IM injection. The drug should be given IV rather than IM in patients with bacteremia, septicemia, or other severe or life-threatening infections and in patients with lowered resistance resulting from debilitating conditions (e.g., malnutrition, trauma, surgery, diabetes, heart failure, malignancy), particularly if shock is present or impending. If an aminoglycoside is administered concomitantly with cefotetan disodium, the drugs should be administered at separate sites. Reconstituted solutions of cefotetan disodium and thawed solutions of the commercially available frozen injection of the drug should be inspected visually for particulate matter and discoloration prior to administration whenever solution and container permit.
Intermittent IV Injection
For direct intermittent IV injection, the contents of vials labeled as containing 1 or 2 g of cefotetan should be reconstituted with 10 or 10-20 mL, respectively, of sterile water for injection to provide solutions containing approximately 97. or 98.-179. mg/mL, respectively. The vials should be shaken until the drug is dissolved and then allowed to stand until the solution is clear. The appropriate dose of reconstituted solution may then be injected directly into a vein over a 3- to 5-minute period.
Intermittent IV Infusion
For intermittent IV infusion, piggyback vials labeled as containing 1 or 2 g of cefotetan may be reconstituted with 50-100 mL of 5% dextrose injection or 0.9% sodium chloride injection to provide solutions containing 10-20 or 20-39 mg/mL, respectively.
Diluted solutions prepared from ADD-Vantage® vials of the drug should be administered only by IV infusion. ADD-Vantage® vials labeled as containing 1 or 2 g of cefotetan should be reconstituted according to the manufacturer’s directions prior to IV infusion.
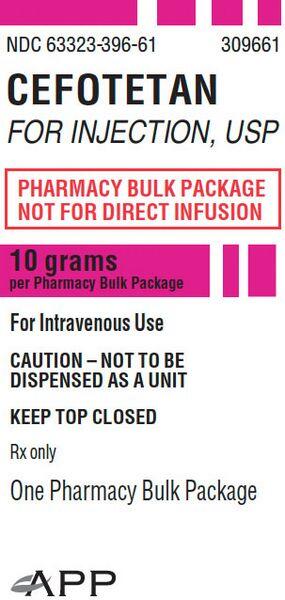
The pharmacy bulk package labeled as containing 10 g of cefotetan should be reconstituted according to the manufacturer’s directions. The pharmacy bulk package is not intended for direct IV infusion; doses of the drug from the reconstituted bulk package must be further diluted in a compatible IV infusion solution prior to administration. Intermittent IV infusions of cefotetan disodium generally have been infused over 20-60 minutes. Cefotetan disodium solutions should preferably be infused IV using butterfly or scalp vein-type needles. Other IV solutions flowing through a common administration tubing or set should be discontinued while cefotetan disodium is being infused. Thawed solutions of the commercially available frozen cefotetan disodium injection in dextrose should be administered only by IV infusion.
Commercially available frozen cefotetan disodium in dextrose injections should not be thawed by warming them in a water bath or by exposure to microwave radiation. A precipitate may form while the commercially available frozen injection in dextrose is frozen; however, this usually will dissolve with little or no agitation upon reaching room temperature, and the potency of the drug is not affected. After thawing at room temperature, the containers should be checked for minute leaks by firmly squeezing the bag.
The injection should be discarded if the container seal or outlet ports are not intact or leaks are found or if the solution is cloudy or contains a precipitate. The injections should not be used in series connections with other plastic containers, since such use could result in air embolism from residual air being drawn from the primary container before administration of fluid from the secondary container is complete.
For further information on administration of the thawed solutions of the commercially available frozen cefotetan disodium in dextrose injections, the manufacturer’s labeling should be consulted.
IM Injection
IM injections of cefotetan disodium are prepared by adding 2 or 3 mL of sterile or bacteriostatic water for injection, 0.9% sodium chloride injection, or 0.5 or 1% lidocaine hydrochloride injection to vials labeled as containing 1 or 2 g of cefotetan, respectively, to provide solutions containing approximately 375 or 471. mg/mL, respectively. IM injections of cefotetan disodium should be made deeply into a large muscle, such as the upper outer quadrant of the gluteus maximus, using usual techniques and precautions. The plunger of the syringe should be drawn back before IM injection to ensure that the needle is not in a blood vessel. Thawed solutions from the commercially available frozen cefotetan disodium injections should not be used for IM administration of the drug.
Dosage
Dosage of cefotetan disodium is expressed in terms of cefotetan. Thawed solutions from the commercially available frozen cefotetan disodium injections should not be used for IM administration of the drug. Adult Dosage The usual adult dosage of cefotetan is 1 or 2 g given IV or IM every 12 hours for 5-21 days; however, the dosage and route of administration should be determined by the type and severity of infection, the susceptibility of the causative organism, and the condition and renal function of the patient. The maximum adult dosage of cefotetan recommended by the manufacturer is 6 g daily.
For the treatment of urinary tract infections, the manufacturer recommends that adults receive 500 mg of cefotetan IV or IM every 12 hours or 1 or 2 g IV or IM every 12 or 24 hours. For the treatment of mild to moderate skin or skin structure infections, the manufacturer recommends that adults receive 2 g of cefotetan IV every 24 hours or 1 g IV or IM every 12 hours; the dosage of cefotetan for these infections caused by Klebsiella pneumoniae should be 1 or 2 g IV or IM every 12 hours.
For the treatment of infections at sites other than the urinary tract, skin, or skin structure, the usual adult dosage is 1 or 2 g IV or IM every 12 hours. However, severe infections in adults may require 2 g given IV every 12 hours and life-threatening infections may require 3 g given IV every 12 hours.
Pelvic Inflammatory Disease
For the treatment of acute pelvic inflammatory disease (PID) in hospitalized patients, adults and adolescents may receive an IV cefotetan dosage of 2 g every 12 hours combined with 100 mg of doxycycline administered IV or orally every 12 hours for at least 2 days after clinical improvement; doxycycline therapy should be continued after the patient is discharged from the hospital in an oral dosage of 100 mg twice daily to complete 10-14 days of therapy.
Perioperative Prophylaxis
If cefotetan is used for perioperative prophylaxis in adults undergoing transurethral surgery, biliary tract surgery, GI surgery, colorectal surgery, appendectomy (nonperforated), or abdominal or vaginal hysterectomy, a single 1- or 2-g dose should be given IV 30-60 minutes prior to surgery. In patients undergoing cesarean section, a single 1- or 2-g dose should be given as soon as the umbilical cord is clamped. If cefotetan is used following contaminated or dirty surgery involving a ruptured abdominal viscus, 1-2 g should be given IV every 6 hours (with or without IV gentamicin in a dosage of 1.5 mg/kg every 8 hour). When used in this situation, the regimen should be continued postoperatively for about 5 days and is considered treatment rather than prophylaxis.
Pediatric Dosage
Although safety and efficacy of cefotetan in children have not been established to date, the American Academy of Pediatrics (AAP) suggests that children older than 1 month of age may receive cefotetan in a dosage of 40-80 mg/kg daily given IV or IM in 2 equally divided doses for the treatment of severe infections.
Dosage in Renal Impairment
In patients with renal impairment, doses and/or frequency of administration of cefotetan should be modified in response to the degree of renal impairment, type and severity of the infection, and susceptibility of the causative organisms. The manufacturer and some clinicians recommend that adults with impaired renal function receive the usual 1- or 2-g dose of cefotetan at the following dosage intervals based on the patient’s creatinine clearance:1, 39 Creatinine Clearance (mL/min) Dosage Interval >30 every 12 h 10-30 every 24 h <10 every 48 h Alternatively, the manufacturer and some clinicians suggest that adults with creatinine clearances of 10-30 mL/minute may receive one-half the usual dose of cefotetan (i.e., 0.5 or 1 g) every 12 hours and that those with creatinine clearances less than 10 mL/minute may receive one-fourth the usual dose (i.e., 250 or 500 mg) every 12 hours.
If this regimen is used, some clinicians suggest that a 1- or 2-g loading dose of cefotetan be given initially. In adults undergoing hemodialysis, the manufacturer recommends that one-fourth the usual dose of cefotetan be given every 24 hours on days between dialysis and one-half the usual dose be given on the day of dialysis.
Cautions
Adverse effects reported with cefotetan are similar to those reported with cephalosporins. For information on adverse effects reported with cephalosporins, see Cautions in the Cephalosporins General Statement and other monographs in 8:12.06. Cefotetan generally is well tolerated; adverse effects have been reported in less than 5% of patients receiving the drug and have required discontinuance of the drug in less than 3% of patients.
Hematologic Effects
Adverse hematologic effects, including eosinophilia, thrombocytosis, thrombocytopenia, neutropenia, leukopenia, agranulocytosis, hemolytic anemia, and positive indirect or direct antiglobulin (Coombs’) test results, have been reported in up to 1.4% of patients receiving cefotetan. Severe hemolytic anemia, including some fatalities, have been reported rarely in association with cefotetan therapy. Hemolytic anemia has been reported in a few women undergoing obstetric and gynecologic procedures who received a single dose of cefotetan for perioperative prophylaxis.
Similar cases of immune-mediated hemolytic anemia have been reported rarely in patients receiving cephalosporins (e.g., cefotaxime, ceftizoxime, ceftriaxone). If a patient develops hemolytic anemia within 2-3 weeks after initiation of cefotetan therapy, the diagnosis of immune-mediated hemolytic anemia should be considered and the drug discontinued until the etiology of the anemia is determined. (See Cautions: Precautions and Contraindications.) Prolongation of bleeding time or prothrombin time (PT), with or without bleeding, has been reported rarely in patients receiving cefotetan (i.e., in 0.14% of patients).
Hypoprothrombinemia also has been reported with other b-lactam antibiotics that contain an N-methylthiotetrazole (NMTT) side chain like that contained in cefotetan (e.g., cefamandole, cefoperazone), and it has been suggested that the NMTT side chain may interfere with hepatic synthesis of vitamin K-dependent clotting factors. Cefotetan does not interfere with adenosine diphosphate-induced, collagen-induced, or arachidonic acid- and epinephrine-induced platelet aggregation.
GI Effects
Adverse GI effects, including diarrhea, nausea, vomiting, and abdominal pain, have been reported in up to 1.5% of patients receiving cefotetan. Hiccups have been reported in at least one patient receiving cefotetan. Colitis has been reported in patients receiving cephalosporins. Clostridium difficile or its toxin was isolated from the feces of several healthy adults who developed diarrhea after receiving a single IV dose of cefotetan.
Clostridium difficile-associated diarrhea and colitis (also known as antibiotic-associated pseudomembranous colitis) caused by overgrowth of toxin-producing clostridia has been reported following cefotetan therapy. C. difficile-associated diarrhea and colitis may range in severity from mild to life-threatening. Mild cases of colitis may respond to discontinuance of cefotetan alone, but diagnosis and management of moderate to severe cases should include sigmoidoscopy (or other appropriate endoscopic examination), appropriate bacteriologic studies, and treatment with fluid, electrolyte, and protein supplementation as indicated.
If colitis is moderate to severe or is not relieved by discontinuance of cefotetan, appropriate anti-infective therapy (e.g., oral metronidazole or vancomycin) should be administered. Isolation of the patient may be advisable. Other causes of colitis also should be considered.
Sensitivity Reactions
Rash, pruritus, anaphylaxis, urticaria, and fever or chills have been reported in up to 1.5% of patients receiving cefotetan. Erythema multiforme (e.g., Stevens-Johnson syndrome) and toxic epidermal necrolysis have been reported in patients receiving cephalosporin therapy. If a hypersensitivity reaction occurs during cefotetan therapy, the drug should be discontinued and the patient treated with appropriate therapy (e.g., IV fluids, IV antihistamines, corticosteroids, vasopressors, and maintenance of an adequate airway and oxygen) as indicated.
Hepatic Effects
Increased serum concentrations of AST (SGOT), ALT (SGPT), alkaline phosphatase, and LDH have been reported in up to 1.2% of patients receiving cefotetan. Hepatic dysfunction, including cholestasis, and increased serum bilirubin concentrations have been reported in patients receiving cephalosporin therapy.
Local Effects
Adverse local effects have been reported in less than 1% of patients receiving cefotetan, and include phlebitis, pain, inflammation, discomfort, and swelling at the injection site. Swelling of the forearm has also been reported. Pain associated with IM injection of the drug may be minimized by administering cefotetan concomitantly with lidocaine.
Renal Effects
Cefotetan does not appear to be nephrotoxic. Although a transient increase in urinary concentrations of total protein occurred in healthy adults who received usual dosages of cefotetan for 3 days, urinary albumin concentrations and excretion of thermophilic aminopeptidase (alanine aminopeptidase), an enzyme originating from renal proximal tubular cells, were generally unaffected, suggesting that the drug does not adversely affect these cells. Nephrotoxicity and increases in BUN and serum creatinine concentrations have been reported in patients receiving cefotetan. Impairment of renal function and toxic nephropathy have been reported in patients receiving cephalosporin therapy.
Although a causal relationship to cefotetan has not been established, interstitial nephritis manifested by fever, rash, pruritus, eosinophilia, hematuria, proteinuria, and azotemia have been reported in at least one patient receiving cefotetan. The nephritis resembled that reported with other anti-infective agents and appeared to be a hypersensitivity reaction to the drug. For more information on anti-infective-induced acute interstitial nephritis, see Cautions: Renal Effects, in the Penicillinase-Resistant Penicillins General Statement 8:12.16.12.
Other Adverse Effects
Several cephalosporins have been associated with seizures, generally when usual dosages of the drugs were not reduced in patients with renal impairment. If seizures occur during cefotetan therapy, the drug should be discontinued and appropriate anticonvulsant therapy administered as indicated. Superinfection, vaginitis, and vaginal candidiasis have been reported in patients receiving cephalosporin therapy.
Precautions and Contraindications
Prior to initiation of cefotetan therapy, careful inquiry should be made concerning previous hypersensitivity reactions to b-lactam antibiotics, including cephalosporins and penicillins, or to other drugs.
There is clinical and laboratory evidence of partial cross-allergenicity among b-lactam antibiotics including penicillins, cephalosporins, and cephamycins. Cefotetan is contraindicated in patients who are hypersensitive to the drug or to cephalosporins and should be used with caution in patients hypersensitive to penicillins.
Because potentially fatal, severe hemolytic anemia has been reported rarely in association with cefotetan therapy, patients who receive prolonged courses of the drug should be monitored periodically for signs and symptoms of hemolytic anemia, including assessment of hematologic parameters, where appropriate.
If a patient develops anemia anytime within 2-3 weeks after administration of cefotetan, the diagnosis of cephalosporin-associated anemia should be considered and the drug stopped until the etiology is determined with certainty.
Blood transfusions may be considered as needed.Cefotetan is contraindicated in individuals who have experienced cephalosporin-associated hemolytic anemia. As with other anti-infective agents, prolonged use of cefotetan may result in overgrowth of nonsusceptible organisms (e.g., enterococci, Pseudomonas, Acinetobacter, Candida). Careful observation of the patient during cefotetan therapy is essential. If superinfection occurs, appropriate therapy should be initiated.
Because Clostridium difficile-associated diarrhea and colitis has been reported with the use of cefotetan, cephalosporins, or other broad-spectrum anti-infective agents, it should be considered in the differential diagnosis of patients who develop diarrhea during cefotetan therapy. Cefotetan should be used with caution in patients with a history of GI disease, especially colitis. Although prolonged prothrombin time (PT) has been reported rarely in patients receiving cefotetan (see Cautions: Hematologic Effects), the PT should be monitored when the drug is used in patients at risk (e.g., patients with renal or hepatic impairment, malnutrition, geriatric patients, patients with cancer), and vitamin K should be administered when indicated.
Patients should be warned to avoid ingestion of alcohol during and for 72 hours after cefotetan therapy because of the possibility that a disulfiram-like reaction may occur. (See Drug Interactions: Alcohol.) Because serum concentrations of cefotetan are higher and more prolonged in patients with renal impairment than in patients with normal renal function, doses and/or frequency of administration of the drug should be decreased in patients with impaired renal function. (See Dosage and Administration: Dosage in Renal Impairment.)
Pediatric Precautions
The manufacturer states that safety and efficacy of cefotetan in children have not been established.
Mutagenicity and Carcinogenicity
In vitro studies have not shown cefotetan to be mutagenic. Studies have not been performed to date to evaluate the carcinogenic potential of the drug.
Pregnancy, Fertitlity and Lactation
Safe use of cefotetan during pregnancy has not been definitely established. Reproduction studies in rats and monkeys using cefotetan dosages up to 20 times the usual human dosage have not revealed evidence of impaired fertility or harm to the fetus. There are no adequate or controlled studies using cefotetan in pregnant women, and the drug should be used during pregnancy only when clearly needed.
Cefotetan has caused adverse effects on the testes of prepubertal rats at high dosages. Reduced testicular weight and seminiferous tubule degeneration occurred in all rats tested following subcutaneous administration of cefotetan in a dosage of 500 mg/kg daily (8-16 times the usual human adult dosage). The drug was given to the rats on days 5-35 of life, the days thought to be developmentally analogous to late childhood and prepuberty in humans. Spermatogonia and spermatocytes were affected, but Sertoli and Leydig cells were unaffected.
The incidence and severity of lesions appeared to be dose dependent since a dosage of 120 mg/kg daily (2-4 times the usual human adult dosage) resulted in only mild degeneration in 110 rats. Adverse effects on testicular development did not occur in rats 7 weeks of age following subcutaneous administration of cefotetan in a dosage up to 1 g/kg daily for 5 weeks or in dogs 3 weeks of age following IV administration of the drug in a dosage up to 300 mg/kg daily for 5 weeks.
Adverse testicular effects (e.g., reduced testicular weight, seminiferous tubule degeneration, delayed maturity of germinal epithelium) have occurred in prepubertal rats receiving other b-lactam antibiotics that contain an N-methylthiotetrazole (NMTT) side chain like that contained in cefotetan (e.g., cefamandole, cefoperazone). The relevance of these findings to humans is unknown. Because cefotetan is distributed into milk, the drug should be used with caution in nursing women.
Drug Interactions
Probenecid
Concomitant administration of oral probenecid does not appear to affect the pharmacokinetics of cefotetan, presumably because cefotetan is eliminated principally by glomerular filtration and nonrenal mechanisms.
Aminoglycosides
In vitro studies indicate that the antibacterial activity of cefotetan and an aminoglycoside may be additive or synergistic against Staphylococcus aureus, Citrobacter, Klebsiella, Enterobacter, Escherichia coli, and Serratia. The combination of cefotetan and an aminoglycoside is generally only additive against Proteus mirabilis and P. vulgaris. The combination of cefotetan and amikacin reportedly does not result in a synergistic effect in vitro against Pseudomonas aeruginosa. Concomitant use of an aminoglycoside and certain cephalosporins reportedly may increase the risk of nephrotoxicity during therapy. Although cefotetan did not potentiate the nephrotoxicity of gentamicin in rats and this effect has not been reported to date in humans, the manufacturer states that nephrotoxicity may be potentiated if the drug is used concomitantly with an aminoglycoside and that renal function should be monitored.
B-Lactam Antibiotics
An additive or synergistic effect has occurred in vitro against some strains of E. coli, E. aerogenes, and Proteus mirabilis when cefotetan was used concomitantly with cefotaxime or piperacillin. The combination of cefotetan and piperacillin reportedly has been antagonistic in vitro against some gram-negative bacteria.
Alcohol
Disulfiram-like reactions characterized by flushing, sweating, headache, and tachycardia may occur if alcohol is ingested within 72 hours after administration of cefotetan. These reactions have been reported with other b-lactam antibiotics that contain an N-methylthiotetrazole (NMTT) side chain similar to that contained in cefotetan (e.g., cefamandole, cefoperazone) and appear to result from accumulation of acetaldehyde.
Laboratory Test Interferences
Tests for Urinary
Glucose Cefotetan may cause false-positive results in urinary glucose determinations using cupric sulfate solutions (e.g., Benedict’s solution, Clinitest®); glucose oxidase methods (e.g., Clinistix®, Tes-Tape®) should be used in patients receiving cefotetan therapy.
Tests for Creatinine
High concentrations of cefotetan may cause falsely elevated serum or urinary creatinine values when the Jaffe reaction is used.
Acute Toxcicity
No information is available on acute overdosage of cefotetan in humans. If acute overdosage of cefotetan occurs, symptomatic treatment should be initiated and hemodialysis considered, especially in patients with renal impairment.
Mechanism of Action
Cefotetan usually is bactericidal in action. Like other b-lactam antibiotics, the antibacterial activity of cefotetan results from inhibition of mucopeptide synthesis in the bacterial cell wall. Studies evaluating the binding of cefotetan to penicillin-binding proteins (PBPs), the target enzymes of b-lactam antibiotics, indicate that the drug has an affinity for and binds to most PBPs of gram-positive bacteria. Cefotetan also has an affinity for and binds to most PBPs of gram-negative bacteria, except PBP 2.Because cefotetan has the highest affinity for PBP 3, the drug usually causes the formation of filamentous forms in susceptible gram-negative bacteria.
Cell lysis and death then occur since cefotetan also has an affinity for PBPs 1a and 1b. Spectrum Although cefotetan is a cephamycin antibiotic, some clinicians classify the drug as a third generation cephalosporin based on its spectrum of activity.
Like third generation cephalosporins, cefotetan usually is less active in vitro against susceptible staphylococci than first generation cephalosporins but has an expanded spectrum of activity against gram-negative bacteria compared with first and second generation cephalosporins. However, most clinicians classify cefotetan as a second generation cephalosporin since the drug generally is less active in vitro on a weight basis than many third generation cephalosporins against gram-negative bacteria and, unlike some currently available third generation cephalosporins, cefotetan generally is inactive against Pseudomonas aeruginosa.
For information on the classification of cephalosporins and closely related b-lactam antibiotics based on spectra of activity, see Spectrum in the Cephalosporins General Statement 8:12.06. In vitro on a weight basis, cefotetan generally is less active than cefotaxime or ceftriaxone against most susceptible organisms including gram-positive cocci, Haemophilus, Neisseria, and Enterobacteriaceae. Cefotetan generally is less active in vitro on a weight basis than cefoxitin against susceptible gram-positive cocci, but generally is more active than cefoxitin against Enterobacteriaceae. The in vitro activity of cefotetan against Bacteroides fragilis is equal to or slightly less than that of cefoxitin.
In Vitro Susceptibility Testing
Inoculum size does not generally affect susceptibility to cefotetan, and MICs for most organisms are generally only 2-4 times greater when the size of the inoculum is increased from 103 to 108 colony-forming units (CFU) per mL. However, MICs for some strains of Morganella, Proteus, and Providencia may be 8 times greater when the inoculum is increased from 103 to 107 CFU/mL. Results of cefotetan in vitro susceptibility tests are generally unaffected by media, pH, or presence of serum.

The National Committee for Clinical Laboratory Standards (NCCLS) states that, if results of in vitro susceptibility testing indicate that a clinical isolate is susceptible to cefotetan, then an infection caused by this strain may be appropriately treated with the dosage of the drug recommended for that type of infection and infecting species, unless otherwise contraindicated. If results indicate that a clinical isolate has intermediate susceptibility to cefotetan, then the strain has a minimum inhibitory concentration (MIC) that approaches usually attainable blood and tissue drug concentrations and response rates may be lower than for strains identified as susceptible.
Therefore, the intermediate category implies clinical applicability in body sites where the drug is physiologically concentrated (e.g., urine) or when a high dosage of the drug can be used. This intermediate category also includes a buffer zone which should prevent small, uncontrolled technical factors from causing major discrepancies in interpretation, especially for drugs with narrow pharmacotoxicity margins. If results of in vitro susceptibility testing indicate that a clinical isolate is resistant to cefotetan, the strain is not inhibited by systemic concentrations of the drug achievable with usual dosage schedules and/or MICs fall in the range where specific microbial resistance mechanisms are likely and efficacy has not been reliably demonstrated in clinical trials. Strains of staphylococci resistant to penicillinase-resistant penicillins should be considered resistant to cefotetan, although routine in vitro susceptibility tests may indicate that the organisms are susceptible to the drug.
Disk Susceptibility Tests
When the disk-diffusion procedure is used to test susceptibility to cefotetan, a disk containing 30 mcg of the drug should be used. When disk-diffusion susceptibility testing is performed according to NCCLS standardized procedures using NCCLS interpretive criteria, Staphylococcus or Enterobacteriaceae with growth inhibition zones of 16 mm or greater are susceptible to cefotetan, those with zones of 13-15 mm have intermediate susceptibility, and those with zones of 12 mm or less are resistant to the drug. When disk-diffusion susceptibility testing is performed according to NCCLS standardized procedures using GC agar (with 1% defined growth supplement), N. gonorrhoeae with growth inhibition zones of 26 mm or greater are susceptible to cefotetan, those with zones of 20-25 mm be have intermediate susceptibility, and those with zones of 19 mm or less are resistant to the drug.
Dilution Susceptibility Tests
When dilution susceptibility testing (agar or broth dilution) is performed according to NCCLS standardized procedures using NCCLS interpretive criteria, Staphylococcus or Enterobacteriaceae with MICs of 16 mcg/mL or less are susceptible to cefotetan, those with MICs of 32 mcg/mL have intermediate susceptibility, and those with MICs of 64 mcg/mL or greater are resistant to the drug. When dilution susceptibility testing of N. gonorrhoeae is performed according to NCCLS standardized procedures using GC agar base (with 1% defined growth supplement), N. gonorrhoeae with MICs of 2 mcg/mL or less are susceptible to cefotetan, those with MICs of 4 mcg/mL have intermediate susceptibility, and those with MICs of 8 mcg/mL or greater are resistant to the drug.
Gram-positive Aerobic Bacteria
Cefotetan’s activity against gram-positive aerobic bacteria generally is similar to that of cefoxitin. Cefotetan generally is active in vitro against penicillinase- and nonpenicillinase-producing strains of Staphylococcus aureus. In addition, most strains of S. pyogenes (group A b-hemolytic streptococci), group B streptococci (e.g., S. agalactiae), and groups C and G streptococci are susceptible to the drug. Cefotetan also is active in vitro against some strains of S. epidermidis and Streptococcus pneumoniae. Enterococci, including E. faecalis (formerly S. faecalis), generally are resistant to the drug. The MIC90 (minimum inhibitory concentration of the drug at which 90% of strains tested are inhibited) of cefotetan for penicillinase- and nonpenicillinase-producing S. aureus is 7.5-16 mcg/mL. The MIC90 of the drug for S. pyogenes and groups B, C, or G streptococci is 2-8 mcg/mL. The MIC50 of cefotetan for S. epidermidis and S. pneumoniae is 1-11. mcg/mL, but the MIC90 of the drug for these organisms ranges from 8-64 mcg/mL or greater and some strains are considered resistant to the drug.
Gram-negative Aerobic Bacteria
Neisseria Cefotetan is active in vitro against Neisseria meningitidis and most strains of penicillinase- and nonpenicillinase-producing Neisseria gonorrhoeae. The MIC90 of cefotetan for N. meningitidis is 0.12 mcg/mL, and the MIC90 of the drug for nonpenicillinase- or penicillinase-producing N. gonorrhoeae is 0.5-4 mcg/mL.
Haemophilus
Cefotetan is active in vitro against most b-lactamase- and non-b-lactamase-producing strains of Haemophilus influenzae. Cefotetan generally is more active in vitro than cefamandole against b-lactamase-producing (ampicillin-resistant) strains of H. influenzae. The MIC90 of cefotetan reported for H. influenzae is 1-4 mcg/mL.
Enterobacteriaceae
Cefotetan generally is active in vitro against the following Enterobacteriaceae: Citrobacter diversus, C. freundii, Enterobacter aerogenes, E. agglomerans, E. cloacae, Escherichia coli, Hafnia alvei, Klebsiella oxytoca, K. ozaenae, K. pneumoniae, Morganella morganii (formerly Proteus morganii), Proteus mirabilis, P. vulgaris, Providencia rettgeri (formerly Proteus rettgeri), P. stuartii, Serratia marcescens, Salmonella, Shigella, and Yersinia enterocolitica. The MIC90 of cefotetan for E. coli, H. alvei, K. oxytoca, K. ozaenae, K. pneumoniae, P. mirabilis, and P. vulgaris is 0.12-4 mcg/mL. The MIC90 of cefotetan for M. morganii, P. rettgeri, P. stuartii, and Y. enterocolitica is 0.25-12 mcg/mL. Although the MIC90 for C. diversus is 0.12-0. mcg/mL, the MIC90 for C. freundii is usually 1-32 mcg/mL. The MIC50 of the drug for Serratia, including S. marcescens, is 0.5-4 mcg/mL, but the MIC90 ranges from 0.5-32 mcg/mL. The in vitro activity of cefotetan against Enterobacter varies considerably, and many strains are considered resistant to the drug. The MIC90 of cefotetan for E. agglomerans is 0.5-32 mcg/mL, but the MIC90 for E. aerogenes or E. cloacae is usually 32 mcg/mL or greater. The MIC90 of cefotetan reported for Salmonella, including S. typhi and S. enteritidis, is 0.05-12. mcg/mL. The MIC90 of cefotetan reported for Shigella, including Sh. sonnei, is 0.06-0.5 mcg/mL.
Pseudomonas
Most strains of Pseudomonas aeruginosa are resistant to cefotetan. Cefotetan has some activity in vitro against Ps. acidovorans, and Ps. stutzeri, and the MIC90 of the drug reported for these organisms is 4-32 mcg/mL. Other Pseudomonas, including Ps. fluorescens, and Ps. putida generally are resistant to cefotetan.
Other Gram-negative Aerobic Bacteria
Cefotetan is active in vitro against some strains of Alcaligenes faecalis (formerly A. odorans) and Moraxella, but Acinetobacter, Achromobacter, and Flavobacterium generally are resistant to the drug. Stenotrophomonas maltophilia (formerly Ps. maltophilia) generally is resistant to cefotetan.
Anaerobic Bacteria
Cefotetan is active in vitro against some gram-positive anaerobic bacteria including Actinomyces, Clostridium, Peptococcus, Peptostreptococcus, and Propionibacterium. The MIC90 of cefotetan reported for most of these gram-positive anaerobes, including Clostridium perfringens and C. botulinum, is 0.06-8 mcg/mL. The MIC90 reported for C. difficile is 16-32 mcg/mL, but many strains of this organism are resistant to the drug. Cefotetan is active in vitro against gram-negative anaerobic bacteria including some strains of Bacteroides, Fusobacterium, andVeillonella. The MIC90 of cefotetan reported for Fusobacterium is 0.13-8 mcg/mL, and the MIC90 for Veillonella is 1-2 mcg/mL. The MIC90 for B. fragilis, B. uniformis, and B. vulgatus is 2-32 mcg/mL. Most strains of B. asaccharolyticus, B. distasonis, B. ovatus, and B. thetaiotaomicron are resistant to cefotetan. Prevotella bivia, P. disiens, and P. melaninogenica (formerly B. bivius, B. disiens, and B. melaninogenicus) may be inhibited in vitro by cefotetan concentrations of 2-32 mcg/mL.
Other Organisms
Cefotetan has some activity in vitro against Mycobacterium fortuitum, but the clinical importance of this in vitro activity has not been determined to date. In one study, 1113 isolates of M. fortuitum were inhibited in vitro by cefotetan concentrations of 50 mcg/mL. Resistance Because cefotetan contains a 7 a-methoxy group on the b-lactam ring, the drug is generally stable against hydrolysis by penicillinases and most cephalosporinases.
Cefotetan is stable against hydrolysis by b-lactamases classified as Richmond-Sykes types I, III (TEM types), IV, and V. The drug is hydrolyzed by PSE 2 b-lactamases produced by Pseudomonas aeruginosa and by some b-lactamases produced by Bacteroides fragilis. Cefotetan is also hydrolyzed by some b-lactamases produced by Enterobacter but is generally more stable than cefoxitin against hydrolysis by cephalosporinases produced by E. coli and E. cloacae.
Resistance to cefotetan in some gram-negative bacteria, including Citrobacter, Enterobacter, and Pseudomonas, apparently is related to permeability factors. Resistance in Bacteroides probably results from nonspecific binding of PBPs and permeability factors. In vitro studies indicate that cefotetan, like cefoxitin, is a potent inducer of b-lactamases and can derepress inducible, chromosomally mediated enzymes in gram-negative bacteria that possess these enzymes.
Cefotetan appears to be active against some strains of Morganella morganii, Providencia stuartii, and Serratia marcescens following derepression of inducible b-lactamases, but Enterobacter and Citrobacter were generally resistant to the drug following derepression.
Pharmacokinetics
In all studies described in the Pharmacokinetics section, cefotetan was administered as cefotetan disodium; dosages and concentrations of the drug are expressed in terms of cefotetan.
Absorption
Cefotetan disodium is not absorbed from the GI tract and must be given parenterally. Following IM administration of a single 0.5- to 2-g dose of cefotetan in healthy adults, the drug appears to be completely absorbed and peak plasma concentrations are attained 1.5-3 hours after the dose. In healthy adults with normal renal function who received a single 0.5-, 1-, or 2-g IM dose of cefotetan, peak plasma cefotetan concentrations averaged 23.3-35,51.9-74, or 91 mcg/mL, respectively, and plasma concentrations 10-12 hours after the dose averaged 4.5, 9-10.15, or 19 mcg/mL, respectively.
Following IV injection over 3-5 minutes of a single 500-mg dose of cefotetan in healthy adults with normal renal function, peak plasma cefotetan concentrations average 79-132 mcg/mL and plasma concentrations average 7.9-8. mcg/mL 8 hours after the dose. In healthy adults with normal renal function, IV injection over 3-5 minutes of a single 1- or 2-g dose of cefotetan results in peak plasma cefotetan concentrations averaging 142-179. or 237 mcg/mL, respectively, and plasma concentrations 9-12 hours after the dose average 7.4-10. or 12-22 mcg/mL, respectively.In one study in healthy adults, free (unbound) plasma cefotetan concentrations declined from a peak of about 50 mcg/mL to about 2 mcg/mL 12 hours after a 2-g IV dose.
Following IV infusion over 30 minutes of a single 1-g dose of cefotetan in healthy adults with normal renal function, peak plasma cefotetan concentrations immediately following completion of the infusion averaged 126-158 mcg/mL and plasma concentrations 11-12 hours later averaged 6.5-9 mcg/mL.
Distribution
Cefotetan is widely distributed into body tissues and fluids including gallbladder, skin, muscle, fat, myometrium, endometrium, fallopian tube, cervix, ovary, uterus and adnexa, prostatic tissue, kidney, ureter, bladder, maxillary sinus mucosa, tonsils, sputum, bile, and wound, prostatic, and peritoneal fluids. The apparent volume of distribution of cefotetan is 8-14. L in healthy adults. In one study in healthy adults, the volume of distribution of cefotetan in the central compartment was 0.136 L/kg and the volume of distribution at steady state was 0.194 L/kg. The volume of distribution of cefotetan reported for adults with impaired renal function does not differ substantially from that reported for patients with normal renal function.
Information on the distribution of cefotetan into CSF is limited, but only low concentrations of the drug are probably attained in CSF after IV administration. Cefotetan is generally distributed into bile, and concentrations in common duct bile are 2-21 times higher than concurrent serum concentrations; concentrations of the drug in gallbladder bile depend on the functional state of the gallbladder. In patients with good gallbladder function who received a single 1-g IV dose of cefotetan, concentrations of the drug in gallbladder bile ranged from 1.3-1. mcg/mL and concentrations in common duct bile ranged from 548 mcg/mL to 1.59 mg/mL in samples obtained 1-4 hours after the dose. Biliary concentrations of the drug are low in patients with poor or absent gallbladder function.
Cefotetan distributes into prostatic fluid in relatively low concentrations, averaging 0.8 mcg/mL after a 1-g IV dose. Cefotetan is 76-91% bound to serum proteins.
The drug is 87.% bound at a concentration of 50 mcg/mL and 76.% bound at a concentration of 400 mcg/mL. Cefotetan crosses the placenta and is distributed into cord blood and amniotic fluid. Peak cefotetan concentrations in umbilical cord serum and amniotic fluid have been reported to be 29 and 8.6 mcg/mL, respectively, following a 1-g IV dose and were attained approximately 3 hours after the dose. The drug is distributed into milk in low concentrations, averaging 0.22, 0.34, and 0.28 mcg/mL 1, 4, and 6 hours, respectively, after a 1-g IV dose.
Elimination
In adults with normal renal function, the distribution half-life of cefotetan (t1/2a) is 0.2-1. hours and the elimination half-life (t1/2b) is 2.8-4.6 hours. Cefotetan does not appear to be metabolized; however, 1-10% of a cefotetan dose is present in plasma and urine as a tautomer of the drug. This tautomer has microbiologic activity and pharmacokinetic properties similar to those of cefotetan.
Following IV or IM administration of a single 0.5- to 2-g dose of cefotetan in adults with normal renal function, 49-81% of the dose is excreted unchanged in urine within 18-24 hours.
Urinary concentrations of the drug are generally highest during the first 1-4 hours following a dose. Cefotetan concentrations average 1.4-2 or 3.5-4 mg/mL in urine collected over the first hour following a single 1- or 2-g dose of the drug, respectively, in healthy adults with normal renal function. Following a single 0.5- or 1-g dose of cefotetan in healthy adults with normal renal function, concentrations of the drug in urine collected over the 12th to 24th hours after the dose average 36-77 mcg/mL. Cefotetan is excreted in urine principally by glomerular filtration, although some renal tubular secretion also occurs.
The principal nonrenal route of elimination of cefotetan is biliary excretion; approximately 20% of a dose is reportedly excreted in bile. Total body clearance of cefotetan from plasma in adults with normal renal function ranges from 29.2-49.7 mL/minute per 1.73 m. Serum concentrations of cefotetan are higher and the serum half-life of the drug is prolonged in patients with impaired renal function. In patients with creatinine clearances of 31-94 mL/minute per 1.73 m, the t1/2b of cefotetan is 3.7-9.1 hours and, in patients with creatinine clearances less than 15 mL/minute per 1.73 m, the t1/2b is 13.1-35.1 hours.
Renal elimination of cefotetan is substantially reduced in patients with impaired renal function; only 5, 8, or 65% of a single 500-mg dose is excreted in urine within 24 hours in patients with creatinine clearances of 0-5, 6-14, or 15-50 mL/minute, respectively. Systemic clearance of cefotetan decreases linearly with decreases in creatinine clearance. Cefotetan is removed by hemodialysis and peritoneal dialysis.
In patients with renal failure undergoing continuous ambulatory peritoneal dialysis who received a single 1-g IV dose of cefotetan, 5-9% of the dose was removed into the dialysate over the 24-hour period immediately following the dose.
Chemistry and Stability
Chemistry
cefotetan Cefotetan is a semisynthetic cephamycin antibiotic derived from oganomycin G, a substance produced by Streptomyces oganonensis. Cephamycins are b-lactam antibiotics that contain a methoxy group rather than a hydrogen at the 7a-position on the b-lactam ring of the cephalosporin nucleus. The methoxy group imparts stability against hydrolysis by many penicillinases and some cephalosporinases. Cefotetan also contains an N-methylthiotetrazole (NMTT) side chain at position 3 of the cephalosporin nucleus similar to that contained in cefamandole and cefoperazone.
The NMTT side chain enhances antibacterial activity, helps to prevent metabolism of the drug, and also may be associated with certain adverse effects (e.g., hypoprothrombinemia, disulfiram-like reactions). Cefotetan is commercially available as the disodium salt. Potency of cefotetan disodium is expressed in terms of cefotetan, calculated on the anhydrous basis. Commercially available cefotetan disodium is a mixture of the R- and S-epimers of the drug; in vivo and in weakly alkaline solutions, a tautomer may be present. The isomers and tautomer have equivalent antibacterial activity.
Cefotetan disodium occurs as a white to pale yellow, lyophilized powder and is very soluble in water and slightly soluble in alcohol, having solubilities of 769 and 1.4 mg/mL in water and alcohol, respectively, at 20°C. The drug has pKas of 2.58 and 3.19. Cefotetan disodium contains approximately 3.5 mEq of sodium per gram of cefotetan. When reconstituted as directed, cefotetan disodium solutions are colorless to yellow and have a pH of 4-6., depending on the concentration of the drug. Cefotetan disodium solutions containing 100 or 200 mg/mL in sterile water for injection have osmolarities of 400-425 or 800 mOsm/L, respectively.
Following reconstitution of 1 or 2 g of the drug with 50-100 mL of 5% dextrose injection or 0.9% sodium chloride injection, solutions containing 10-39 mg/mL are slightly hypertonic, having osmolarities of 340-480 mOsm/L depending on the concentration. When reconstituted as directed, cefotetan disodium solutions for IM injection containing 375 or 471. mg/mL are extremely hypertonic, having osmolarities greater than 1500 mOsm/L.
The commercially available frozen cefotetan disodium in dextrose injections are sterile, nonpyrogenic, iso-osmotic solutions of the drug and have osmolalities of approximately 300 mOsm/kg; about 1.9 or 1.1 g of dextrose has been added to the 1- or 2-g injections of cefotetan, respectively, to adjust osmolality. Cefotetan disodium in dextrose frozen injections also contain hydrochloric acid and/or sodium bicarbonate to adjust pH to 4-6.; sodium bicarbonate neutralizes cefotetan free acid to the disodium salt.
Stability
Cefotetan disodium sterile powder should be stored at 22°C or less and protected from light, and is stable for 24 months after the date of manufacture when stored under these conditions. Cefotetan disodium powder and solutions of the drug may darken (i.e., to a deeper yellow) with age depending on storage conditions; however, this color change does not indicate loss of potency. Following reconstitution with sterile water for injection, cefotetan disodium solutions containing 95-182 mg of cefotetan per mL are stable for 24 hours at 25°C, 96 hours when refrigerated at 5°C, or at least 1 week when frozen at -20°C.
Piggyback vials containing 1 or 2 g of cefotetan that have been reconstituted with 50-100 mL of 5% dextrose injection or 0.9% sodium chloride injection are stable for 24 hours at 25°C or 96 hours at 5°C. When reconstituted as directed in 0.9% sodium chloride injection or 5% dextrose injection, solutions prepared from ADD-Vantage® vials of the drug are stable for 24 hours at room temperature (25°C); these solutions should not be kept in a refrigerator or frozen. The manufacturer states that ADD-Vantage® vials of cefotetan should be reconstituted only when the patient is ready to receive the drug.
Following reconstitution with sterile or bacteriostatic water for injection, 0.9% sodium chloride injection, or 0.5 or 1% lidocaine hydrochloride injection, solutions containing approximately 400 or 500 mg/mL are stable for 24 hours at 25°C, 96 hours at 5°C, or at least 1 week when frozen at -20°C. Reconstituted cefotetan disodium solutions that have been transferred to disposable glass or plastic syringes are stable for 24 hours at room temperature or 96 hours when refrigerated.Frozen cefotetan disodium solutions should be thawed at room temperature and should not be refrozen. If stored at -20°C, cefotetan disodium is stable for at least 4 weeks in plasma and at least 5.5 weeks in urine. The manufacturer states that the stability of the commercially available frozen cefotetan disodium injection may vary.
These injections are stable for at least 90 days from the date of shipment when stored at -20°C. The frozen injection should be thawed at room temperature or under refrigeration and, once thawed, should not be refrozen. Thawed solutions of the commercially available frozen injection are stable for 48 hours at room temperature (25°C) or 21 days when refrigerated at 5°C. The commercially available frozen injection of the drug in dextrose is provided in a plastic container fabricated from specially formulated multilayered plastic PL 2040 (Galaxy®).
Solutions in contact with the plastic can leach out some of its chemical components in very small amounts within the expiration period of the injection; however, safety of the plastic has been confirmed in tests in animals according to USP biological tests for plastic containers as well as tissue culture toxicity studies. Cefotetan disodium is physically incompatible with tetracyclines, aminoglycosides, and heparin. Cefotetan disodium should not be admixed with any of these incompatible drugs since admixing may result in clouding of the solution and/or formation of a precipitate.
Preparations
Cefotetan Disodium Parenteral For injection 1 g (of cefotetan) Cefotan®, AstraZeneca 2 g (of cefotetan) Cefotan®, AstraZeneca 10 g (of cefotetan) pharmacy Cefotan®, bulk package AstraZeneca For injection, for 1 g (of cefotetan) Cefotan® ADD-Vantage®, IV infusion AstraZeneca Cefotan® Piggyback, AstraZeneca 2 g (of cefotetan) Cefotan® ADD-Vantage®, AstraZeneca Cefotan® Piggyback, AstraZeneca Cefotetan Disodium in Dextrose Parenteral Injection, 20 g (of cefotetan) per mL Cefotan® in Iso-osmotic (frozen) for IV (1 g) in 3.8% Dextrose Dextrose Injection, (Galaxy® infusion only [Baxter]) AstraZeneca 40 g (of cefotetan) per mL Cefotan® in Iso-osmotic (2 g) in 2.2% Dextrose Dextrose Injection, (Galaxy® [Baxter]) AstraZeneca

