Cefoperazone is a semisynthetic, third generation cephalosporin antibiotic.
Uses
Cefoperazone is used in the treatment of intra-abdominal infections (including peritonitis), urinary tract infections, respiratory tract infections, skin and skin structure infections, septicemia, and gynecologic infections (including pelvic inflammatory disease [PID] and endometritis) caused by susceptible organisms.
Prior to initiation of cefoperazone therapy, appropriate specimens should be obtained for identification of the causative organism and in vitro susceptibility tests. Cefoperazone may be started pending results of susceptibility tests but should be discontinued if the causative organism is found to be resistant to the drug. In serious infections when the causative organism is unknown, concomitant therapy with an aminoglycoside may be indicated pending results of in vitro susceptibility tests.
The manufacturer recommends that, if cefoperazone is used concomitantly with an aminoglycoside, in vitro susceptibility tests should be performed to determine the combined activity of the drugs and renal function should be monitored, especially in patients with impaired renal function.
Gram-positive Aerobic Bacterial Infections
Cefoperazone is used in adults for the treatment of lower respiratory tract infections caused by susceptible Staphylococcus aureus, Streptococcus, or S. pyogenes (group A b-hemolytic streptococci); urinary tract infections caused by susceptible enterococci; skin and skin structure infections (including cellulitis) caused by susceptible S. aureus or group A b-hemolytic streptococci; gynecologic infections caused by susceptible S. epidermidis or S. agalactiae (group B streptococci); or septicemia caused by susceptible S. aureus, S. pneumoniae, or group B streptococci.
Most clinicians state that cefoperazone generally should not be used in the treatment of infections caused by gram-positive bacteria when a penicillin or a first generation cephalosporin could be used.
Although cefoperazone reportedly has been effective in a limited number of patients for the treatment of peritonitis and other intra-abdominal infections, skin and skin structure infections, gynecologic infections such as endometritis or PID, or urinary tract infections in which enterococci were isolated (usually as a component of a polymicrobial infection), most strains of enterococci are moderately resistant or resistant to the drug and other anti-infectives generally are preferred; therefore, cefoperazone should be used with caution in these infections and only at dosages that would be expected to achieve adequate concentrations of the drug.
Gram-negative Aerobic Bacterial Infections
Cefoperazone is used in adults for the treatment of lower respiratory tract infections caused by susceptible Haemophilus influenzae, Enterobacter, Escherichia coli, Klebsiella pneumoniae, Proteus mirabilis, or Pseudomonas aeruginosa; urinary tract infections caused by susceptible E. coli or Ps. aeruginosa; septicemia caused by susceptible E. coli, Klebsiella (including K. pneumoniae), Proteus, or Ps. aeruginosa; peritonitis and other intra-abdominal tract infections caused by susceptible E. coli or Ps. aeruginosa; skin or skin structure infections caused by susceptible Ps. aeruginosa; or gynecologic infections such as endometritis or pelvic inflammatory disease (PID) caused by susceptible E. coli or Neisseria gonorrhoeae.
However, in vitro studies indicate that cefoperazone is less active on a weight basis than cefotaxime, ceftizoxime, and ceftriaxone against susceptible Enterobacteriaceae, and other cephalosporins (e.g., cefepime, cefotaxime, ceftazidime, ceftriaxone, ceftizoxime) generally are preferred when a parenteral cephalosporin is indicated for the treatment of infections known or suspected to be caused by Enterobacteriaceae. Although cefoperazone is active in vitro against some strains of Ps. aeruginosa and is more active against these organisms than many other available cephalosporins, cefoperazone is not generally considered a drug of choice for the treatment of infections caused by Ps. aeruginosa.
Because most strains of Ps. aeruginosa are only susceptible to high concentrations of cefoperazone in vitro, an aminoglycoside should be used in conjunction with cefoperazone if the drug is used in the treatment of infections known or suspected to be caused by this organism.
Anaerobic and Mixed Aerobic-Anaerobic Bacterial Infections
Cefoperazone is used in adults for the treatment of peritonitis and other intra-abdominal infections caused by susceptible anaerobic gram-negative bacilli (including Bacteroides fragilis); septicemia caused by susceptible Clostridium or anaerobic gram-positive cocci; or gynecologic infections such as endometritis or pelvic inflammatory disease (PID) caused by susceptible Clostridium, Bacteroides (including B. fragilis), or anaerobic gram-positive cocci.
Cefoperazone has been effective when used alone in the treatment of mixed aerobic-anaerobic infections including intra-abdominal infections and gynecologic infections such as endometritis and PID. However, cefoperazone is not generally considered a drug of choice for the treatment of intra-abdominal infections and is not included in current US Centers for Disease Control and Prevention (CDC) guidelines for the treatment of PID. Because cefoperazone, like most other cephalosporins, has no activity against Chlamydia, an anti-infective regimen effective against C. trachomatis should be used in addition to cefoperazone if the drug is used in the treatment of PID and C. trachomatis is one of the suspected pathogens.
Perioperative Prophylaxis
Cefoperazone has been used for perioperative prophylaxis in a limited number of patients undergoing abdominal hysterectomy or coronary artery bypass surgery. However, studies indicate that cefoperazone is no more effective than first or second generation cephalosporins for perioperative prophylaxis and should therefore not be used prophylactically when these drugs could be used.
Other anti-infectives (e.g., cefazolin, cefotetan, cefoxitin) usually are the preferred drugs for perioperative prophylaxis. Some clinicians state that third generation cephalosporins (e.g., cefoperazone, cefotaxime, ceftriaxone, ceftazidime, ceftizoxime) and fourth generation cephalosporins (e.g., cefepime) should not be used for perioperative prophylaxis since they are expensive, some are less active than cefazolin against staphylococci, they have a spectrum of activity that is wider than necessary for organisms encountered in elective surgery, and their use for prophylaxis promotes emergence of resistant organisms.
Dosage and Administration
Reconstitution and Administration
Cefoperazone sodium is administered by IV infusion or by deep IM injection. Although cefoperazone has been injected directly into a vein over a 3- to 5-minute period in some studies, the manufacturer does not recommend rapid, direct IV injection of the drug. Cefoperazone sodium sterile powder for injection should be reconstituted only with a compatible IV solution. Solutions should be allowed to stand following reconstitution to allow any foaming to dissipate and permit visual inspection for complete dissolution. Vigorous and prolonged agitation may be necessary to dissolve cefoperazone sodium in concentrations greater than 333 mg/mL; the maximum solubility of the drug in compatible IV solutions at 15-30°C is approximately 475 mg/mL.
Intermittent or Continuous IV Infusion
For intermittent IV infusion, vials labeled as containing 1 or 2 g of cefoperazone should initially be reconstituted with a minimum of 2.8 mL of compatible IV solution per g of the drug; the manufacturer recommends that 5 mL of a compatible IV solution be used per g of cefoperazone. The entire quantity of resulting solution should then be withdrawn from the vial and further diluted in 20-40 mL of a compatible IV solution per g of cefoperazone. Alternatively, piggyback units containing 1 or 2 g of cefoperazone may be reconstituted with 20-40 or 40-80 mL, respectively, of a compatible IV solution; if 5% dextrose and lactated Ringer’s injection or lactated Ringer’s injection is used as the diluent for administration, the drug should be initially reconstituted with 2.8-5 mL of another compatible IV solution per g of the drug.
The pharmacy bulk package labeled as containing 10 g of cefoperazone should be reconstituted according to the manufacturer’s directions.
The pharmacy bulk package is not intended for direct IV infusion; doses of the drug from the reconstituted bulk package must be further diluted in a compatible IV infusion solution prior to administration.
Thawed solutions of the commercially available frozen cefoperazone sodium injection should be administered only by intermittent or continuous IV infusion. After thawing at room temperature, the container should be checked for minute leaks by firmly squeezing the bag. The injection should be discarded if the container seal is not intact or leaks are found or if the solution is cloudy or contains a precipitate.
Additives should not be introduced into the injection container. The injection should not be used in series connections with other plastic containers, since such use could result in air embolism from residual air being drawn from the primary container before administration of fluid from the secondary container is complete. Intermittent IV infusions of cefoperazone sodium should be infused over 15-30 minutes. For continuous IV infusion, reconstituted cefoperazone solutions should be further diluted to a final concentration of 2-25 mg/mL. If an aminoglycoside is administered concomitantly with cefoperazone, the drugs should be administered at separate sites.
IM Injection
Although sterile water for injection, bacteriostatic water for injection (containing benzyl alcohol or parabens), or another compatible IV solution may be used alone as a diluent to prepare IM injections of cefoperazone, the manufacturer recommends that a lidocaine hydrochloride solution be used as the diluent when IM injections having a final concentration of 250 mg/mL or greater are to be administered.
A 2-step dilution procedure using sterile water for injection and 2% lidocaine hydrochloride injection should be followed to prepare IM injections with a final concentration of 250 mg/mL or greater.
Vial labeled as Final cefoperazone Step 1 volume of Step 2 volume of containing (g of concentration sterile water to 2% lidocaine HCL cefoperazone) be added to be added 1 g 333 mg/mL 2 mL 0.6 mL 250 mg/mL 2.8 mL 1 mL 2 g 333 mg/mL 3.8 mL 1.2 mL 250 mg/mL 5.4 mL 1.8 mL
When this 2-step procedure is used, the specified volume of sterile water for injection should be added to the vial of cefoperazone, the vial should be gently agitated until the drug is completely dissolved, and then the specified volume of 2% lidocaine hydrochloride should be added to the vial. Solutions prepared in this manner contain approximately 0.5% lidocaine hydrochloride.
Alternatively, if lidocaine hydrochloride is not used as the diluent, IM injections of cefoperazone may be prepared by adding 2.6 mL of sterile water for injection, bacteriostatic water for injection (containing benzyl alcohol or parabens), or another compatible IV solution to a vial labeled as containing 1 g of cefoperazone or by adding 5 mL of one of these diluents to a vial labeled as containing 2 g of the drug to provide solutions containing 333 mg/mL. To provide solutions containing 250 mg/mL, 3.8 or 7.2 mL of one of these diluents may be added to a vial labeled as containing 1 or 2 g of the drug, respectively. IM injections prepared using bacteriostatic water for injection containing benzyl alcohol should not be used in neonates. (See Cautions: Pediatric Precautions.)
Dosage
Dosage of cefoperazone sodium is expressed in terms of cefoperazone and is identical for IM or IV administration.
Adult Dosage
The usual adult dosage of cefoperazone is 2-4 g daily given in equally divided doses every 12 hours.
The manufacturer states that for the treatment of severe infections or infections caused by less susceptible organisms, the dose and/or frequency of administration may be increased.
Cefoperazone has been administered in dosages of 6-12 g daily given in 2, 3, or 4 equally divided doses. In one pharmacokinetic study in severely immunocompromised adults, a dosage of 16 g daily was administered by continuous IV infusion without evidence of complications.
Pediatric Dosage
Although safe use of cefoperazone in children younger than 12 years of age has not been definitely established, the American Academy of Pediatrics (AAP) recommends a dosage of 100-150 mg/kg daily given in 2 or 3 divided doses for the treatment of mild to moderate infections in pediatric patients older than 1 month of age. Duration of Therapy The duration of cefoperazone therapy depends on the type of infection but should generally be continued for at least 48-72 hours after the patient becomes afebrile or evidence of eradication of the infection is obtained.
Although other anti-infectives are preferred, if cefoperazone is used in the treatment of infections caused by Streptococcus pyogenes (group A b-hemolytic streptococci), therapy should be continued for at least 10 days to decrease the risk of rheumatic fever or glomerulonephritis.
Dosage in Renal and Hepatic Impairment
In adults with hepatic disease and/or biliary obstruction, dosage of cefoperazone generally should not exceed 4 g daily. If higher dosage is used in these patients, serum concentrations of cefoperazone should be monitored. Modification of the usual dosage of cefoperazone is generally unnecessary in patients with impaired renal function; however, if high dosage is used in these patients, serum concentrations of cefoperazone should be monitored and dosage decreased if there is evidence of accumulation of the drug.
In adults with both hepatic and substantial renal impairment, dosage of cefoperazone should not exceed 1-2 g daily unless serum concentrations of the drug are monitored. In patients undergoing hemodialysis, although the serum half-life of the drug is only slightly reduced, the manufacturer states that the dosing regimen should be timed so that a dose of cefoperazone is scheduled at the end of the dialysis period.
Cautions
Adverse effects reported with cefoperazone are similar to those reported with other cephalosporins. In addition, hypoprothrombinemia and disulfiram-like reactions also have been reported with cefoperazone.
Dermatologic and Sensitivity Reactions
Hypersensitivity reactions, including rash, skin reactions, fever, eosinophilia, urticaria, and pruritus, have been reported in less than 2% of patients receiving cefoperazone. Positive direct antiglobulin (Coombs’) test results have also been reported occasionally; however, it is not clear whether the mechanism of this reaction is immunologic in nature. If a severe hypersensitivity reaction occurs during cefoperazone therapy, the drug should be discontinued and patient given appropriate therapy (e.g., epinephrine, corticosteroids, maintenance of an adequate airway, oxygen) as indicated.
Hematologic Effects
Slight decreases in hemoglobin concentration and hematocrit value have been reported in 5% or less of patients receiving cefoperazone. Reversible neutropenia has also been reported in about 2% of patients receiving prolonged administration of the drug. Cefoperazone has caused hypoprothrombinemia, with or without bleeding, and vitamin K deficiency. The manufacturer states that vitamin K deficiency during cefoperazone therapy may be due in part from cefoperazone-induced reduction in vitamin K-producing bacteria in the GI tract. Hypoprothrombinemia also has been reported with other b-lactam antibiotics that contain an N-methylthiotetrazole (NMTT) side chain like that contained in cefoperazone (e.g., cefamandole, cefotetan), and it has been suggested that the NMTT side chain may interfere with hepatic synthesis of vitamin K-dependent clotting factors.
Hypoprothrombinemia and bleeding during cefoperazone therapy have been reported most frequently in geriatric or debilitated patients, patients with severe renal failure, or following radical GI surgery and have usually been reversed by administration of vitamin K.
Cefoperazone-induced hypoprothrombinemia may be more likely to occur in the presence of hypoalbuminemia. Patients with poor nutritional status, malabsorption states (e.g., cystic fibrosis), or alcohol dependence or those receiving prolonged enteral or parenteral hyperalimentation are at particular risk of cefoperazone-induced vitamin K deficiency.
GI Effects
Adverse GI effects, including diarrhea or loose stools, nausea, and vomiting, have been reported in patients receiving cefoperazone. Diarrhea has occurred in 0.5-7% of patients receiving the drug. Most reported cases of diarrhea were mild or moderate in severity and responded to symptomatic therapy or discontinuance of the drug; however, severe diarrhea and colitis have been reported rarely.
Clostridium difficile has been isolated from the feces of patients who developed diarrhea while receiving cefoperazone. Mild cases of C. difficile-associated diarrhea and colitis may respond to discontinuance of cefoperazone alone, but diagnosis and management of moderate to severe cases should include sigmoidoscopy (or other appropriate endoscopic examination), appropriate bacteriologic studies, and treatment with fluid, electrolyte, and protein supplementation as indicated. If C. difficile-associated diarrhea and colitis is moderate to severe or is not relieved by discontinuance of cefoperazone, appropriate anti-infective therapy (e.g., oral metronidazole or vancomycin) should be administered. Isolation of the patient may be advisable.
Other causes of colitis should be considered.
Hepatic Effects
Mild, transient elevations of serum AST (SGOT), ALT (SGPT), and alkaline phosphatase concentrations have been reported in 5-10% of patients receiving cefoperazone; however, these elevations in liver enzymes were not accompanied by overt signs or symptoms of hepatic dysfunction and their clinical importance has not been established. One patient with a history of liver disease developed substantially elevated liver enzymes and clinical signs and symptoms of nonspecific hepatitis during therapy with cefoperazone; however, the enzymes returned to pretreatment concentrations and the symptomatology resolved following discontinuance of the drug.
Renal Effects
Transient elevations in BUN and serum creatinine concentrations have been reported in up to 6% of patients receiving cefoperazone.
Local Effects
Transient pain at the injection site reportedly occurs in 0.7-2% of patients receiving cefoperazone IM, and phlebitis reportedly occurs in 0.8-2% of patients receiving the drug IV.
Other Adverse Effects
Headache, dizziness, tremulousness, and chills have been reported rarely in patients receiving cefoperazone.
Precautions and Contraindications
Prior to initiation of cefoperazone therapy, careful inquiry should be made concerning previous hypersensitivity reactions to cephalosporins, penicillins, or other drugs. There is clinical and laboratory evidence of partial cross-allergenicity among cephalosporins and other b-lactam antibiotics, including penicillins and cephamycins.
Cefoperazone is contraindicated in patients who are hypersensitive to the drug or other cephalosporins and should be used with caution in patients with a history of hypersensitivity to penicillins.
Use of cephalosporins should be avoided in patients who have had an immediate-type (anaphylactic) hypersensitivity reaction to penicillins. Although it has not been definitely proven that allergic reactions to antibiotics are more frequent in atopic individuals, the manufacturer states that cefoperazone should be used with caution in patients with a history of allergy, particularly to drugs.
Prolonged use of cefoperazone may result in overgrowth of nonsusceptible organisms. Careful observation of the patient during cefoperazone therapy is essential. If suprainfection or superinfection occurs, appropriate therapy should be instituted. Cefoperazone should be used with caution in patients with a history of GI disease, particularly colitis. Because C. difficile-associated diarrhea and colitis has been reported with the use of cephalosporins, it should be considered in the differential diagnosis of patients who develop diarrhea during cefoperazone therapy.
Because hypoprothrombinemia, with or without bleeding, and vitamin K deficiency have occurred rarely in patients receiving cefoperazone, prothrombin time (PT) should be monitored when the drug is used in patients receiving prolonged enteral or parenteral hyperalimentation or in patients with poor nutritional status, malabsorption states (e.g., cystic fibrosis), or alcohol dependence. Vitamin K should be administered if indicated.

The manufacturer states that prophylactic vitamin K therapy in patients receiving cefoperazone is probably not warranted. However, some clinicians suggest that prophylactic vitamin K may be indicated when cefoperazone is used in geriatric or debilitated patients or patients with impaired renal and/or liver function.
Patients should be warned to avoid ingestion of alcohol during and for 72 hours after cefoperazone therapy since disulfiram-like reactions have been reported with the drug. (See Drug Interactions: Alcohol.) Because serum concentrations of cefoperazone are higher and more prolonged in patients with hepatic disease and/or biliary obstruction, serum concentrations of cefoperazone should be monitored in these patients when dosage of the drug is greater than 4 g daily.
Serum concentrations of cefoperazone should also be monitored when dosage of the drug is greater than 1-2 g daily in patients with both hepatic and renal impairment. Although modification of the usual dosage of cefoperazone is generally unnecessary in patients with impaired renal function, serum concentrations of cefoperazone should be monitored if high dosage of the drug is used in these patients and dosage decreased if evidence of accumulation occurs. (See Dosage and Administration: Dosage in Renal and Hepatic Impairment.)
Pediatric Precautions
The manufacturer states that safety and efficacy of cefoperazone in children younger than 12 years of age have not been established. Because of reported toxicity of benzyl alcohol in neonates, IM injections of cefoperazone prepared using bacteriostatic water for injection containing benzyl alcohol should not be used in neonates.
Mutagenicity and Carcinogenicity
Animal and in vitro studies have not shown cefoperazone to be mutagenic at the chromosomal or subchromosomal level. Studies have not been performed to date to evaluate the carcinogenic potential of cefoperazone.
Pregnancy, Fertitlity and Lactation
Reproduction studies in mice, rats, and monkeys using cefoperazone dosages up to 10 times the usual human dosage have not revealed evidence of impaired fertility or harm to the fetus. There are no adequate and controlled studies to date using cefoperazone in pregnant women, and the drug should be used during pregnancy only when clearly needed. Cefoperazone has caused adverse effects on the testes of prepubertal rats. Reduced germinal cell population and vacuolation of Sertoli cell cytoplasm occurred following subcutaneous administration of cefoperazone in a dosage of 1000 mg/kg daily (approximately 16 times the average adult human dosage).
The severity of lesions was dosage dependent in the range of 100-1000 mg/kg daily; the low dosage caused a minor reduction in spermatocytes. The effect on spermatocytes has not been observed in adult rats. The cefoperazone-induced lesions were histologically reversible at all but the highest dosage levels; however, the studies did not evaluate subsequent development of reproductive function.
Adverse testicular effects (e.g., reduced testicular weight, seminiferous tubule degeneration, delayed maturity of germinal epithelium) have occurred in prepubertal rats receiving other b-lactam antibiotics that contain an N-methylthiotetrazole (NMTT) side chain like that contained in cefoperazone (e.g., cefamandole, cefotetan). The relevance of these findings to humans is not known. Because cefoperazone is distributed into milk, the drug should be used with caution in nursing women.
Drug Interactions
Alcohol
Disulfiram-like reactions characterized by flushing, headache, nausea, vomiting, sweating, and tachycardia have occurred when alcohol was ingested within 72 hours after administration of cefoperazone. Symptoms usually occur within 15-30 minutes after ingestion of alcohol and subside 1-2 hours later. These reactions do not occur if alcohol is ingested prior to the first dose of cefoperazone.
Disulfiram-like reactions have been reported with other b-lactam antibiotics that contain an N-methylthiotetrazole (NMTT) side chain similar to that contained in cefoperazone (e.g., cefamandole, cefotetan) and appear to result from accumulation of acetaldehyde. Ingestion of alcohol should be avoided during and for 72 hours after the administration of cefoperazone.
Aminoglycosides
In vitro studies indicate that the antibacterial activity of cefoperazone and aminoglycosides may be additive or synergistic against some gram-negative bacilli including Pseudomonas aeruginosa and Serratia marcescens; however, synergy is unpredictable. The manufacturer recommends that, when concomitant therapy with an aminoglycoside and cefoperazone is considered, in vitro susceptibility tests be performed to determine the combined activity of the drugs. Concurrent use of aminoglycosides and certain cephalosporins reportedly may increase the risk of nephrotoxicity during therapy. Although this has not been reported to date with cefoperazone, the manufacturer states that renal function should be monitored in patients, especially those with impaired renal function, receiving the drug concomitantly with an aminoglycoside.
Clavulanic Acid
In vitro studies using cefoperazone and clavulanic acid, a b-lactamase inhibitor, showed synergism of the combination against many Enterobacteriaceae, Ps. aeruginosa, Staphylococcus aureus, and Bacteroides fragilis.
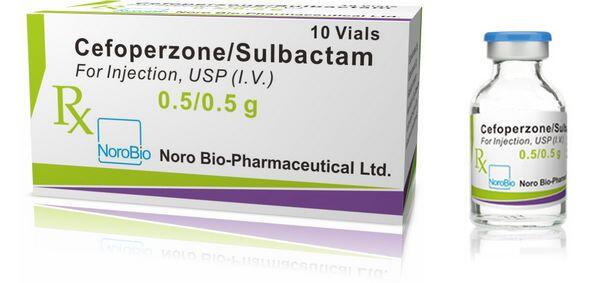
Sulbactam
Results of in vitro studies indicate that the combination of cefoperazone and sulbactam results in synergistic bactericidal effects against many strains of b-lactamase-producing gram-positive and gram-negative bacteria, including Staphylococcus, Escherichia coli, Proteus, Ps. aeruginosa, Acinetobacter, and Bacteroides. Sulbactam is a b-lactamase inhibitor that has a high affinity for and irreversibly binds to certain b-lactamases that can inactivate b-lactam antibiotics. A 1:1 fixed-ratio combination of cefoperazone with sulbactam (not commercially available in the US) has been effective when used parenterally for the treatment of a variety of respiratory tract, urinary tract, or skin and skin structure infections caused by b-lactamase-producing bacteria, including S. aureus, S. epidermidis, Escherichia coli, Enterobacter, Klebsiella, and Pseudomonas.
Laboratory Test Interferences
Immunohematology Tests
Positive direct antiglobulin (Coombs’) test results have been reported in a few patients receiving cefoperazone. This reaction may interfere with hematologic studies or transfusion cross-matching procedures.
Tests for Urinary Glucose
Like most other cephalosporins, cefoperazone reportedly causes false-positive results in urine glucose determinations using cupric sulfate solution (Benedict’s reagent, Fehlings reagent, Clinitest®).
Mechanism of Action
Cefoperazone usually is bactericidal in action. Like other cephalosporins, the antibacterial activity of the drug results from inhibition of mucopeptide synthesis in the bacterial cell wall. For information on the mechanism of action of cephalosporins, see Mechanism of Action in the Cephalosporins General Statement 8:12.06. The target enzymes of b-lactam antibiotics have been classified as penicillin-binding proteins (PBPs) and appear to vary substantially among bacterial species.
Studies evaluating the binding of cefoperazone to PBPs indicate that the drug has a high affinity for PBPs 1, 2, and 3 of Escherichia coli and PBPs 1a and 3 of Pseudomonas aeruginosa. Spectrum Based on its spectrum of activity, cefoperazone is classified as a third generation cephalosporin. For information on the classification of cephalosporins and closely related b-lactam antibiotics based on spectra of activity, see Spectrum in the Cephalosporins General Statement 8:12.06.
Like other currently available parenteral third generation cephalosporins (e.g., cefotaxime, ceftazidime, ceftizoxime, ceftriaxone), cefoperazone generally is less active in vitro against susceptible staphylococci than a first generation cephalosporin but has an expanded spectrum of activity against gram-negative bacteria compared with first and second generation cephalosporins. T
he spectrum of activity of cefoperazone resembles that of other parenteral third generation cephalosporins. However, in vitro on a weight basis, cefoperazone is less active than cefotaxime, ceftizoxime, or ceftriaxone against most Enterobacteriaceae but is more active than these drugs against Pseudomonas aeruginosa.
In Vitro Susceptibility Testing
Results of in vitro cefoperazone susceptibility tests for some gram-negative bacilli (especially Bacteroides fragilis, Citrobacter, Escherichia coli, Klebsiella, Serratia, and Pseudomonas aeruginosa) may be greatly affected by the size of the inoculum.
Although pH of the in vitro media may also affect results of cefoperazone susceptibility tests, activity of the drug is not generally influenced if the pH is 5.5-8. The National Committee for Clinical Laboratory Standards (NCCLS) states that, if results of in vitro susceptibility testing indicate that a clinical isolate is susceptible to cefoperazone, then an infection caused by this strain may be appropriately treated with the dosage of the drug recommended for that type of infection and infecting species, unless otherwise contraindicated.
If results indicate that a clinical isolate has intermediate susceptibility to cefoperazone, then the strain has a minimum inhibitory concentration (MIC) that approaches usually attainable blood and tissue drug concentrations and response rates may be lower than for strains identified as susceptible. Therefore, the intermediate category implies clinical applicability in body sites where the drug is physiologically concentrated (e.g., urine) or when a high dosage of the drug can be used.
This intermediate category also includes a buffer zone which should prevent small, uncontrolled technical factors from causing major discrepancies in interpretation, especially for drugs with narrow pharmacotoxicity margins. If results of in vitro susceptibility testing indicate that a clinical isolate is resistant to cefoperazone, the strain is not inhibited by systemic concentrations of the drug achievable with usual dosage schedules and/or MICs fall in the range where specific microbial resistance mechanisms are likely and efficacy has not been reliably demonstrated in clinical trials. Strains of staphylococci resistant to penicillinase-resistant penicillins should be considered resistant to cefoperazone, although results of in vitro susceptibility tests may indicate that the organisms are susceptible to the drug.
Disk Susceptibility Tests
When the disk-diffusion procedure is used to test susceptibility to cefoperazone, a disk containing 75 mcg of cefoperazone should be used. The cephalosporin class disk containing 30 mcg of cephalothin or disks containing other cephalosporins should not be used for testing susceptibility to cefoperazone. When disk-diffusion susceptibility testing is performed according to NCCLS standardized procedures using NCCLS interpretive criteria, Staphylococcus, Enterobacteriaceae, Pseudomonas aeruginosa, or Acinetobacter with growth inhibition zones of 21 mm or greater are susceptible to cefoperazone, those with zones of 16-20 mm have intermediate susceptibility, and those with zones of 15 mm or less are resistant to the drug.
Dilution Susceptibility Tests
When dilution susceptibility testing (agar or broth dilution) is performed according to NCCLS standardized procedures using NCCLS interpretive criteria, Staphylococcus, Enterobacteriaceae, and Ps. aeruginosa and other non-Enterobacteriaceae gram-negative bacilli (e.g., other Pseudomonas spp., Acinetobacter, Stenotrophomonas maltophilia) with MICs of 16 mcg/mL or less are susceptible to cefoperazone, those with MICs of 32 mcg/mL have intermediate susceptibility, and those with MICs of 64 mcg/mL or greater are resistant to cefoperazone.
Gram-positive Aerobic Bacteria
In vitro, cefoperazone concentrations of 4 mcg/mL inhibit most strains of Staphylococcus aureus and S. epidermidis. Cefoperazone is active in vitro against most penicillinase-producing S. aureus; however, strains of staphylococci resistant to penicillinase-resistant penicillins also generally are resistant to cefoperazone. In vitro, cefoperazone concentrations of 2 mcg/mL or less inhibit most strains of groups A and B streptococci, viridans streptococci, and Streptococcus pneumoniae.
Cefoperazone has some in vitro activity against enterococci including E. faecalis (formerly S. faecalis), S. faecium, and S. durans, and the MIC50 (minimum inhibitory concentration of the drug at which 50% of strains tested are inhibited) of cefoperazone reported for E. faecalis is 16-64 mcg/mL. However, cefoperazone is much less active than acylaminopenicillins (mezlocillin, piperacillin) against enterococci and many strains of these organisms are considered resistant to cefoperazone. Although in vitro cefoperazone concentrations of 25 mcg/mL reportedly inhibit some strains of Listeria monocytogenes, most strains of the organism are considered resistant to the drug.
Gram-negative Aerobic Bacteria
Generally, cefoperazone is active against the following Enterobacteriaceae: Citrobacter diversus, C. freundii, Enterobacter aerogenes, E. cloacae, Escherichia coli, Klebsiella oxytoca, K. pneumoniae, Morganella morganii (formerly Proteus morganii), Proteus mirabilis, P. vulgaris, Providencia, Salmonella, Shigella, and Yersinia enterocolitica. The MIC90 of cefoperazone for most Enterobacteriaceae is 0.5-8 mcg/mL; however, the MIC90 of the drug for C. freundii, E. cloacae, and Providencia is usually 8-16 mcg/mL.
Although some strains of Serratia are inhibited in vitro by cefoperazone concentrations of 16 mcg/mL, most strains of this organism are resistant to the drug. In vitro on a weight basis, cefoperazone is more active than cefotaxime, ceftizoxime or ceftriaxone against Pseudomonas, including Ps. aeruginosa; however, cefoperazone is less active against these organisms than is ceftazidime. The MIC90 of cefoperazone for Ps. aeruginosa is reportedly 8-50 mcg/mL.
Cefoperazone is active in vitro against Haemophilus influenzae (including ampicillin-resistant strains) and H. parainfluenzae. The MIC90 of cefoperazone reported for H. influenzae is 0.25-1 mcg/mL. Cefoperazone is also active in vitro against Neisseria gonorrhoeae (including penicillinase-producing strains) and N. meningitidis, and the MIC90 of the drug for both penicillinase-producing and nonpenicillinase-producing strains of N. gonorrhoeae is reportedly 0.01-0. mcg/mL. Cefoperazone also has some activity against Bordetella pertussis. Acinetobacter are generally resistant to cefoperazone.
Anaerobic Bacteria
Cefoperazone is active in vitro against many anaerobic bacteria including Bifidobacterium, Eubacterium, Fusobacterium, Peptococcus, Peptostreptococcus, Propionibacterium, and Veillonella. Cefoperazone is generally active in vitro against Clostridium, including some strains of C. difficile. In one study, susceptible anaerobic bacteria were generally inhibited in vitro by cefoperazone concentrations of 1-8 mcg/mL. Some strains of Bacteroides are inhibited in vitro by cefoperazone concentrations of 8-32 mcg/mL; however, cefoperazone concentrations of 16-64 mcg/mL or higher are generally required in vitro to inhibit B. fragilis. In vitro, cefoperazone is less active than cefoxitin, clindamycin, chloramphenicol, or piperacillin against B. fragilis.
Resistance
For information on possible mechanisms of bacterial resistance to cephalosporins, see Resistance in the Cephalosporins General Statement 8:12.06. Cefoperazone is more susceptible to inactivation by b-lactamases than are cefoxitin, cefotaxime, ceftizoxime, and cefuroxime. Cefoperazone is generally resistant to inactivation by b-lactamases that act principally as cephalosporinases and is not generally hydrolyzed by enzymes produced by Ps. aeruginosa or S. aureus. However, cefoperazone may be inactivated by certain TEM and SHV-1 type b-lactamases, Richmond-Sykes type 1 cephalosporinases, and type III and IV penicillinases. Cefoperazone is also generally hydrolyzed by a b-lactamase produced by B. fragilis. Although partial cross-resistance has been reported between cefoperazone and cefotaxime, cross-resistance among the third generation cephalosporins is unpredictable.
Pharmacokinetics
In all studies described in the Pharmacokinetics section, cefoperazone was administered as the sodium salt; dosages and concentrations of the drug are expressed in terms of cefoperazone.
Absorption
Cefoperazone is not appreciably absorbed from the GI tract and must be given parenterally. Following IM administration of a single 1- or 2-g dose of cefoperazone in healthy adults, peak serum concentrations of the drug are attained within 1-2 hours and average 65-74 and 97-111 mcg/mL, respectively. Serum concentrations of cefoperazone average 7 mcg/mL 8 hours after the 1-g IM dose and 14 mcg/mL 8 hours after the 2-g IM dose. Following IV administration over 15 minutes of a single 1-, 2-, 3-, or 4-g dose of cefoperazone in healthy adults, serum concentrations of the drug average 153, 253, 340, and 506 mcg/mL, respectively, at the end of the infusion and 0.5, 2, 2, and 6 mcg/mL, respectively, 12 hours later.
When 2 g of cefoperazone is administered IV over 30 minutes to healthy adults, serum concentrations of the drug average 232. mcg/mL immediately at the end of the infusion, 92.8 mcg/mL 1 hour later, 18.7 mcg/mL 4 hours later, and 1.2 mcg/mL 12 hours later. In one study in neonates 1-2 days of age who received a single cefoperazone dose of 50 mg/kg given by IV injection over 3 minutes, serum concentrations of the drug averaged 109 mcg/mL 30 minutes after completion of the infusion, 97 mcg/mL 2 hours later, 56 mcg/mL 8 hours later, and 13 mcg/mL 24 hours later. A single 0.5- to 1-g dose of cefoperazone in children younger than 5 years of age reportedly resulted in peak serum concentrations of the drug ranging from 60-100 mcg/mL.
Distribution
Following IM or IV administration, cefoperazone is widely distributed into body tissues and fluids including ascitic fluid, bile, sputum, endometrium, myometrium, tonsils, sinus mucous membranes, middle ear fluid, lungs, pleural fluid, prostatic tissue, adipose tissue, aqueous humor, and bone. The apparent volume of distribution of cefoperazone is approximately 10-13 L in adults and 0.5 L/kg in neonates. Cefoperazone concentrations in CSF are low following IM or IV administration of usual dosages of the drug in patients with uninflamed meninges.
CSF concentrations of the drug are generally higher in patients with inflamed meninges and appear to correlate directly with total CSF leukocyte counts and CSF protein concentrations. In one study in adults with inflamed meninges receiving cefoperazone IV in a dosage of 100 mg/kg 1 or 3 times daily, CSF concentrations of the drug ranged from 0-11. mcg/mL. Following IV administration of a cefoperazone dose of 50 mg/kg in neonates 2-3 weeks of age, CSF concentrations of cefoperazone in samples taken 1-4 hours after the dose ranged from 2.8-9 or 1.1-7 mcg/mL in neonates with or without meningitis, respectively.
Concentrations of cefoperazone in bile following IM or IV administration of usual dosages of the drug are generally up to 100 times higher than concurrent serum concentrations. In patients with T-tubes and relatively normal hepatic function, peak concentrations of cefoperazone in bile reportedly range from 675 mcg/mL to 6.1 mg/mL. Following rapid IV injection of a single 2-g dose of cefoperazone, biliary concentrations of the drug reportedly are 66 mcg/mL and 6 mg/mL 0.5 and 3 hours after the injection, respectively. Although concentrations of cefoperazone in bile are lower in patients with biliary or hepatocellular disease, therapeutic biliary concentrations of the drug may be attained. In vitro studies indicate that the degree of protein binding of cefoperazone depends on the concentration of the drug.
Cefoperazone is 93% bound to serum proteins at a concentration of 25 mcg/mL, 90% bound at 250 mcg/mL, and 82% bound at 500 mcg/mL.
Cefoperazone crosses the placenta. Peak cefoperazone concentrations in umbilical cord blood generally occur 1 hour after administration of the drug to the mother. Following a single 1- or 2-g dose of cefoperazone, amniotic fluid concentrations of the drug reportedly are 2.8-4.8 mcg/mL1, 2 and umbilical cord blood concentrations are 25 mcg/mL. Cefoperazone is distributed in low concentrations into milk, and concentrations of the drug in milk reportedly range from 0.4-0.9 mcg/mL following IV administration of a single 1-g dose.
Elimination
The serum half-life of cefoperazone in adults with normal renal and hepatic function reportedly ranges from 1.6-2.6 hours. In patients with hepatic impairment, the serum half-life of cefoperazone is prolonged and urinary excretion of the drug is increased. In one study in patients with severe biliary tract obstruction or cirrhosis, the serum half-life of cefoperazone ranged from 3.4-7. hours.
The serum half-life, peak serum concentrations, and area under the concentration-time curve (AUC) of cefoperazone reported for patients with impaired renal function are not substantially different than those reported for patients with normal renal function. The serum half-life of cefoperazone in children 2 months to 11 years of age reportedly averages 2.2 hours, and the half-life of the drug in neonates reportedly ranges from 6-12 hours.
Half-life of cefoperazone in neonates depends principally on gestational and chronologic age. In one study, the half-life of cefoperazone averaged 7.2 hours in full-term neonates, 7.6 in premature neonates with a gestational age of 33-36 weeks, and 8.9 hours in premature neonates with a gestational age of less than 33 weeks. Cefoperazone is excreted principally in bile. Following IM or IV administration of a single dose of cefoperazone, approximately 15-30% of the dose is excreted in urine as unchanged drug within 12-24 hours; less than 1% of the dose is excreted in urine as metabolites. A
lthough at least 6 in vitro degradation products of cefoperazone have been identified, some with antibacterial activity, only 2 metabolites of the drug have been identified in urine. In patients with severe hepatic disease or biliary obstruction, renal excretion of cefoperazone is increased and up to 90% of a dose may be excreted in urine in these patients.
Cefoperazone is excreted in urine by glomerular filtration and, to a lesser extent, by tubular secretion. In patients with normal renal and hepatic function, concentrations of cefoperazone in urine reportedly may be greater than 2.2 mg/mL following a 15-minute IV infusion of a single 2-g dose of the drug and almost 1 mg/mL after a single 2-g IM dose of the drug.
The serum clearance of cefoperazone in adults with normal renal and hepatic function is reportedly 75-96.3 mL/minute per 1.73 m. Because cefoperazone is excreted principally by nonrenal mechanisms, concomitant administration of probenecid has only a slight effect on serum concentrations or serum half-life of the drug. Cefoperazone is removed by hemodialysis.
There is no published information on the effect of peritoneal dialysis on cefoperazone.
Chemistry and Stability
Chemistry
Cefoperazone is a semisynthetic cephalosporin antibiotic. The major structural difference between cefoperazone and other parenteral cephalosporins is that cefoperazone contains a piperazine side chain; this side chain results in antipseudomonal activity. Cefoperazone also contains an N-methylthiotetrazole (NMTT) side chain at position 3 of the cephalosporin nucleus similar to that contained in cefamandole and cefotetan. The NMTT side chain enhances antibacterial activity, helps to prevent metabolism of the drug, and also may be associated with certain adverse effects (e.g., hypoprothrombinemia, disulfiram-like reactions).
Cefoperazone is commercially available as the sodium salt. Potency of cefoperazone sodium is expressed in terms of cefoperazone. Cefoperazone sodium occurs as a white, crystalline powder. The drug is freely soluble in water and poorly soluble in alcohol.
The drug has a pKa of 2.55. Cefoperazone sodium has a maximum solubility of approximately 475 mg/mL in compatible IV solutions at 15-30°C; prolonged and vigorous agitation may be required to dissolve the drug at concentrations greater than 333 mg/mL. The sodium salt of cefoperazone contains 1.5 mEq of sodium per gram of cefoperazone. Reconstituted solutions of cefoperazone sodium are colorless to straw-colored and have a pH of 4.5-6.5, depending on the concentration of the drug.
Commercially available frozen cefoperazone sodium injections containing 1 or 2 g of cefoperazone in 4.6 or 3.6% dextrose injection, respectively, are sterile solutions of the drug and have osmolalities of approximately 300 mOsm/kg; sodium hydroxide and/or hydrochloric acid may have been added to adjust pH to 4.5-6.5.
Stability
Commercially available cefoperazone sodium sterile powder for injection should be stored at 25°C or less and protected from light. It is unnecessary to protect reconstituted solutions of cefoperazone sodium from light.
The commercially available frozen cefoperazone sodium injection should be stored at a temperature not greater than -20°C. Cefoperazone sodium is chemically and physically compatible with the following IV solutions: sterile water for injection, bacteriostatic water for injection containing benzyl alcohol or parabens, 0.9% sodium chloride, 5% dextrose, 5% dextrose and lactated Ringer’s, 5% dextrose and 0.2% or 0.9% sodium chloride, 10% dextrose, lactated Ringer’s, 0.5% or 2% lidocaine hydrochloride, Normosol® M and 5% dextrose, or Normosol® R. When stored at 15-25°C or 2-8°C, reconstituted solutions of cefoperazone sodium may be stored in glass or plastic syringes, or in glass or flexible plastic parenteral solution containers.
When stored at -20 to -10°C, reconstituted solutions of cefoperazone sodium may be stored in plastic syringes or flexible plastic parenteral solution containers.
Following reconstitution in sterile water for injection, bacteriostatic water for injection (containing benzyl alcohol or parabens), or 0.5% lidocaine hydrochloride injection, cefoperazone sodium solutions containing approximately 300 mg of cefoperazone per mL are stable for 24 hours at 15-25°C or 5 days at 2-8°C. In concentrations of 2-50 mg/mL, cefoperazone sodium is chemically and physically stable for 24 hours at 15-25°C or 5 days at 2-8°C in the following IV solutions: 5% dextrose, 5% dextrose and 0.2% or 0.9% sodium chloride, Normosol® M and 5% dextrose, or Normosol® R. In concentrations of 2-50 mg/mL, the drug also is stable for 24 hours at 15-25°C in 5% dextrose and lactated Ringer’s injection or 10% dextrose injection.
In concentrations of 2-300 mg/mL, the drug is stable for 24 hours at 15-25°C or 5 days at 2-8°C in 0.9% sodium chloride injection and, in a concentration of 2 mg/mL, the drug is stable under the same conditions in lactated Ringer’s. Following reconstitution with sterile water for injection or 0.9% sodium chloride injection, cefoperazone sodium solutions containing approximately 300 mg of cefoperazone per mL are stable for 5 weeks when stored at -20 to -10°C.
Extemporaneously prepared cefoperazone sodium solutions containing 50 mg of cefoperazone per mL in 5% dextrose injection or solutions containing 2 mg of cefoperazone per mL in 5% dextrose and 0.2% or 0.9% sodium chloride injection are stable for 3 weeks when stored at -20 to -10°C.
Frozen solutions of cefoperazone sodium should be thawed at room temperature. The manufacturer states that frozen solutions of cefoperazone should not be thawed using microwave techniques.
Once thawed, unused portions should be discarded and should not be refrozen. Cefoperazone sodium pharmacy bulk packages that have been reconstituted with sterile water for injection to a concentration of 100 mg/mL of cefoperazone are stable for 24 hours at room temperature or 5 days when refrigerated; individual doses of these reconstituted solutions should be transferred to compatible IV infusion solutions as soon as possible following reconstitution of the pharmacy bulk package.
The manufacturer states that the stability of the commercially available frozen cefoperazone sodium injection containing 1 g (20 mg/mL) or 2 g (40 mg/mL) may vary. These injections are stable for at least 90 days from the date of shipment when stored at -20°C.
The frozen injections should be thawed at room temperature and, once thawed, should not be refrozen. Thawed solutions of the commercially available frozen injection are stable for 48 hours at room temperature (25°C) or 10 days when refrigerated at 5°C. The commercially available frozen injections of the drug are provided in a plastic container fabricated from specially formulated polyvinyl chloride (PVC).
Solutions in contact with the plastic can leach out some of its chemical components in very small amounts (e.g., bis(2-ethylhexyl)phthalate [BEHP, DEHP]in up to 5 ppm) within the expiration period of the injection; however, safety of the plastic has been confirmed in tests in animals according to USP biological tests for plastic containers as well as by tissue culture toxicity studies.
Cefoperazone sodium is potentially physically and/or chemically incompatible with some drugs, including aminoglycosides, but the compatibility depends on several factors (e.g., concentrations of the drugs, specific diluents used, resulting pH, temperature). Specialized references should be consulted for specific compatibility information. Because of the potential for incompatibility, the manufacturer states that cefoperazone sodium and aminoglycosides should not be admixed. For further information on chemistry, mechanism of action, spectrum, resistance, pharmacokinetics, uses, cautions, drug interactions, laboratory test interferences, and dosage and administration of cefoperazone, see the Cephalosporins General Statement 8:12.06
Preparations
Cefoperazone Sodium Parenteral For injection 1 g (of cefoperazone) Cefobid®, Pfizer 2 g (of cefoperazone) Cefobid®, Pfizer 10 g (of cefoperazone) Cefobid®, pharmacy bulk package Pfizer For injection, for 1 g (of cefoperazone) Cefobid® Piggyback, IV infusion Pfizer 2 g (of cefoperazone) Cefobid® Piggyback, Pfizer Cefoperazone Sodium in Dextrose Parenteral Injection (frozen) 20 mg (of cefoperazone) per Cefobid® in Iso-osmotic , for IV infusion mL (1 g) in 4.6% Dextrose Dextrose Injection, (Galaxy® [Baxter]) Pfizer 40 mg (of cefoperazone) per Cefobid® in Iso-osmotic mL (2 g) in 3.6% Dextrose Dextrose Injection, (Galaxy® [Baxter]) Pfizer

