Drug Nomenclature
Pharmacopoeias
In Europe, Japan, and US.
European Pharmacopoeia, 6th ed., 2008 and Supplements 6.1 and 6.2 (Nalidixic Acid).
An almost white or pale yellow, crystalline powder. Practically insoluble in water; slightly soluble in alcohol and in acetone; soluble in dichloromethane. It dissolves in dilute solutions of alkali hydroxides. Store in airtight containers. Protect from light.
The United States Pharmacopeia 31, 2008 (Nalidixic Acid).
A white to very pale yellow, odourless crystalline powder. Very slightly soluble in water and in ether; soluble 1 in 910 of alcohol and 1 in 29 of chloroform; slightly soluble in acetone, in methyl alcohol, and in toluene; soluble in dichloromethane and in solutions of fixed alkali hydroxides and carbonates. Store in airtight containers.
Adverse Effects
The most frequent adverse reactions to nalidixic acid involve the gastrointestinal tract, skin, and CNS. Gastrointestinal effects have been reported in about 8% of patients and include nausea, vomiting, diarrhoea, and abdominal pain.
Adverse effects on the skin include photosensitivity reactions with erythema and bullous eruptions, allergic rashes, urticaria, and pruritus. Erythema multiforme and Stevens-Johnson syndrome have been reported rarely. Eosinophilia, fever, angioedema, and, rarely, anaphylactoid reactions have occurred. Neurological effects include visual disturbances, headache, dizziness or vertigo, drowsiness, and sometimes confusion, depression, excitement, and hallucinations.
Toxic psychoses or convulsions have occurred, especially after large doses; convulsions are most likely in patients with predisposing factors such as cerebral arteriosclerosis or epilepsy. There have been reports of intracranial hypertension, especially in infants and young children, and also of metabolic acidosis. Peripheral neuropathies, muscular weakness, and myalgia are occasional adverse effects.
Sixth cranial nerve palsy has been reported rarely. Arthralgia has been reported (degenerative changes in weight-bearing joints of young animals are documented). Tendon damage has occasionally been associated with nalidixic acid and related compounds, the fluoroquinolones (see Effects on the Musculoskeletal System, under Ciprofloxacin). Cholestatic jaundice, thrombocytopenia, and leucopenia have occurred rarely, as has haemolytic anaemia in patients who may or may not have G6PD deficiency. There have been isolated reports of fatal auto-immune haemolytic anaemia in elderly patients.
Precautions
Nalidixic acid is contra-indicated in patients with a history of convulsive disorders and in those with severe renal impairment. It should be given with care to patients with hepatic or moderate renal impairment, severe cerebral arteriosclerosis, or G6PD deficiency. Blood counts and renal and hepatic function should be monitored if treatment continues for more than 2 weeks. It should be avoided in infants less than 3 months old.
Since nalidixic acid and related antimicrobials have been shown to cause degenerative changes in weight-bearing joints of young animals, it has been suggested that these compounds should not generally be used in patients aged under 18 years, pregnant women, or during breast feeding (but see also below) unless the benefits outweigh the risks. Treatment should be stopped if symptoms of neuropathy or arthralgia occur.
Tendon damage may occur rarely and treatment should be stopped if patients experience tendon pain, inflammation, or rupture. Exposure to strong sunlight or sunlamps should be avoided during treatment with nalidixic acid. Nalidixic acid may cause false-positive reactions in urine tests for glucose using copper reduction methods.
Breast feeding
The American Academy of Pediatrics states that nalidixic acid is usually compatible with breast feeding, although haemolytic anaemia has been reported in a breast-fed infant, with no evidence of G6PD deficiency, whose mother had received nalidixic acid.
Porphyria
Nalidixic acid has been associated with acute attacks of porphyria and is considered unsafe in porphyric patients.
Interactions
The absorption of nalidixic acid is reduced by sucralfate, and divalent and trivalent cations such as aluminium, calcium, iron, magnesium, and zinc, and therefore use of nalidixic acid with antacids, iron preparations, or other preparations containing such cations, whether as active ingredients or excipients, may result in subtherapeutic serum concentrations of the antibacterial. It is recommended that such products should not be given within 2 hours before or after nalidixic acid.
The excretion of nalidixic acid is reduced and plasma concentrations increased by probenecid.
Other antibacterials such as chloramphenicol, nitrofurantoin, and tetracycline have been shown to antagonise the action of nalidixic acid in vitro and should not be used together. Fatal haemorrhagic enterocolitis has been associated with the use of nalidixic acid and high-dose intravenous melphalan in children; use with other alkylating antineoplastics is also contra-indicated.
There is a possible risk of increased nephrotoxicity when nalidixic acid is given with ciclosporin. Nalidixic acid is reported to enhance the effect of oral anticoagulants such as warfarin; this may be due in part to displacement of anticoagulant from its plasma binding sites. The dose of anticoagulant may need to be reduced. The effect of some quinolone antibacterials on xan-thines is discussed under Caffeine, and Theophylline.
Convulsions may be precipitated by the use of some quinolones with NSAIDs (see Analgesics, under Interactions of Ciprofloxacin), although this has not been reported with nalidixic acid.
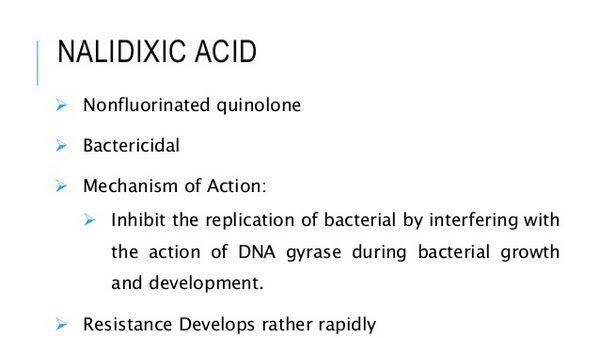
Antimicrobial Action
Nalidixic acid is considered to act by interfering with the replication of bacterial DNA, probably by inhibiting DNA gyrase (topoisomerase) activity. It is active against Gram-negative bacteria including Escherichia coli, Klebsiella spp., Proteus spp., Enterobacter spp., Salmonella spp., and Shigella spp., and is usually bactericidal. Pseudomonas aeruginosa, Gram-positive bacteria, and anaerobes are not generally susceptible. Bacterial resistance may develop rapidly, sometimes within a few days of commencing treatment, but it does not appear to be transferable or R-plasmid mediated (see also below).
Cross-resistance occurs with oxolinic acid and cinoxacin. The antibacterial activity of nalidixic acid is not significantly affected by differences in urinary pH. Antagonism between nalidixic acid and other antibacterials such as chloramphenicol, nitrofurantoin, and tetracycline has been shown in vitro.
Resistance
Bacterial plasmid-mediated resistance to quinolones had not been seen by the late 1980s. A report of such resistance to nalidixic acid in Shigella dysenteriae responsible for an epidemic of shigellosis in Bangladesh in 1987, was questioned at the time. On reinspection of the data, chromosomal mutation rather than plasmid-mediated resistance was confirmed as the mechanism responsible so far for resistance to quinolones. Subsequent data in an isolate of Klebsiella pneumoniae has, however, suggested that plasma-mediated resistance to quinolones may be possible.
Pharmacokinetics
Nalidixic acid is rapidly and almost completely absorbed from the gastrointestinal tract, and peak plasma concentrations of 20 to 40 micrograms/mL have been reported 1 to 2 hours after a 1-g oral dose. Plasma half-lives of about 1 to 2.5 hours have been reported (but see below).
Nalidixic acid is partially metabolised to hydroxynali-dixic acid, which has antibacterial activity similar to that of nalidixic acid and accounts for about 30% of active drug in the blood. About 93% of nalidixic acid and 63% of hydroxynalidixic acid are bound to plasma proteins.
Both nalidixic acid and hydroxynalidixic acid are rapidly metabolised to inactive glucuronide and di-carboxylic acid derivatives; the major inactive metabolite 7-carboxynalidixic acid is usually only detected in urine. Nalidixic acid and its metabolites are excreted rapidly in the urine, nearly all of a dose being eliminated within 24 hours.
More than 80% of the drug excreted in the urine is as inactive metabolites, but peak urinary concentrations of active drug averaging about 150 to 200 micrograms/mL are achieved 3 to 4 hours after a single 1-g dose. Hydroxynalidixic acid accounts for about 80 to 85% of activity in the urine. Urinary excretion is reduced by probenecid. About 4% of a dose is excreted in the faeces.
Traces of nalidixic acid are distributed into breast milk and appear to cross the placenta. Although a plasma half-life of 1 to 2.5 hours is generally cited for nalidixic acid, values of 6 to 7 hours have been reported for active drug (nalidixic acid and hydroxynalidixic acid) after using more specific and sensitive assay techniques and longer sampling periods than previously.
The elimination rate of nalidixic acid appears to be not markedly altered by renal impairment, but the elimination of hydroxynalidixic acid is significantly reduced. 7-Carboxynalidixic acid has appeared in the plasma of patients with renal impairment. Plasma concentrations of active drug were higher and the half-life prolonged in elderly subjects.
Uses and Administration
Nalidixic acid is a 4-quinolone antibacterial used in the treatment of uncomplicated lower urinary-tract infections due to Gram-negative bacteria other than Pseudomonas spp.. It has also been used to treat shigellosis (bacillary dysentery).
The usual dose is about 4 g daily in 4 divided oral doses for 7 to 14 days in acute infections, reducing thereafter to half this dose in chronic infections. Since bacterial resistance may develop rapidly it has been suggested that if treatment with nalidixic acid has not resulted in a negative urine culture within 48 hours another antimicrobial should be used. For details of reduced doses in renal impairment, see below. For details of doses in infants and children, see below.
Although the antibacterial activity of nalidixic acid does not appear to be influenced by urinary pH, the use of sodium bicarbonate or sodium citrate does increase the concentration of active drug in the urine.
Commercial preparations containing nalidixic acid, sodium bicarbonate, and sodium citrate have been used in some countries. It is also used with the analgesic phenazopyridine.
Administration in children
Although nalidixic acid is not generally recommended for use in patients under 18 years of age, it is licensed in both the UK and the USA for infants and children over 3 months of age. The usual oral dose is 55 to 60 mg/kg daily in 4 divided doses for at least 7 days, reducing thereafter to about 30 mg/kg daily in 4 divided doses for prolonged treatment (but see Precautions, above). In addition, the BNFC suggests that a dose of 30 mg/kg daily in 2 divided doses may be given for prophylaxis of urinary-tract infections.
Administration in renal impairment
In the UK, some products of nalidixic acid have been licensed for use at half the usual dose in patients with a creatinine clearance below 20 mL/minute (the BNFC suggests a similar reduction in children with creatinine clearance 20 mL/minute per 1.73 m or less). However, other licensed product information does not include this information and suggests that nalidixic acid should not be used in patients with severe renal impairment.
Preparations
British Pharmacopoeia 2008: Nalidixic Acid Oral Suspension; Nalidixic Acid Tablets; The United States Pharmacopeia 31, 2008: Nalidixic Acid Oral Suspension; Nalidixic Acid Tablets.
Proprietary Preparations
Argentina: Nalidix; Wintomylon; Brazil: Naluril; Wintomylon; Canada: NegGrarrr; Chile: Wintomylon; France: Negram; Greece: Nalacid; Hong Kong: Wintomylon; Hungary: Nevigramon; India: Diarlop; Gramoneg; Negadix; Indonesia: Urineg; Ireland: Negram; Israel: NegGram; Italy: Betaxina Nalidixin; Naligram; NegGram; Uri-Flor; Mexico: A-N-Dix; Acidix; Fardixon; Kamilon; Nalix; Pronal Dix; Seltomylon; Urlix; Uronalin; Wintomylon; Poland: Nevigramon; Portugal: Wintomilon; Russia: Negram; South Africa: Puromylon; Winlorrylon; United Kingdom (UK): Negram; Uriben; United States of America (US or USA): NegGram.
Multi-ingredient
Ireland: Mictral; Mexico: Azo-Uronalin; Azo-Wintomylon; Azogen; Nalixone; Naxilan-Plus; Pirifur
| Dosage forms of Nalidixic Acid: |
|---|
| Nalidixic acid powder |
Therapeutic classes of Nalidixic Acid:
Anti-Infective Agents, Enzyme Inhibitors, Nucleic Acid Synthesis Inhibitors


 (2 votes, average: 4.50 out of 5)
(2 votes, average: 4.50 out of 5)